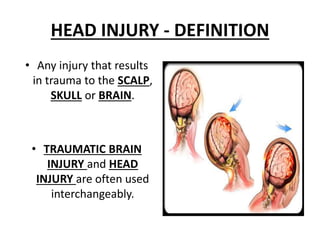
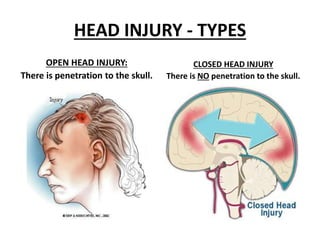
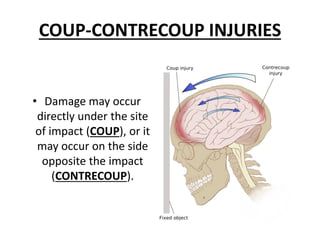
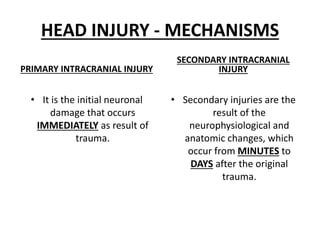
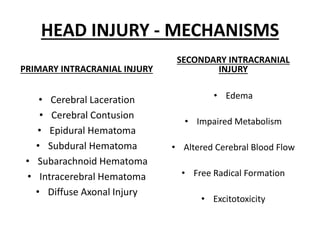
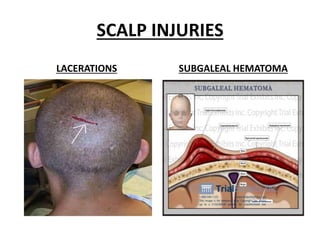
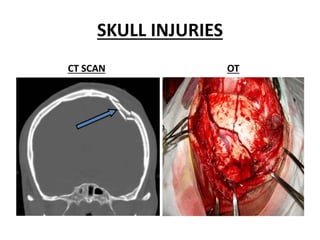
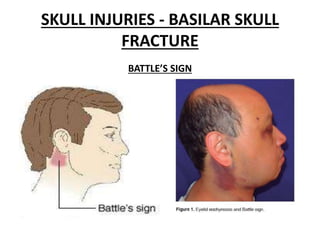
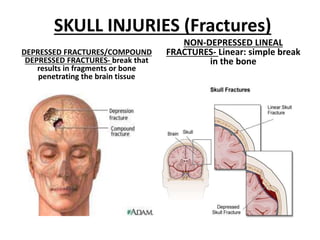
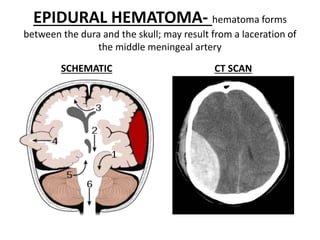
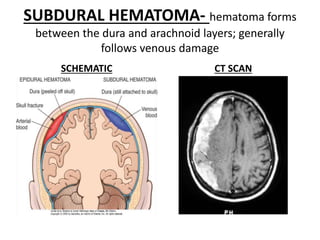
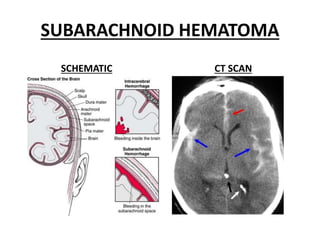
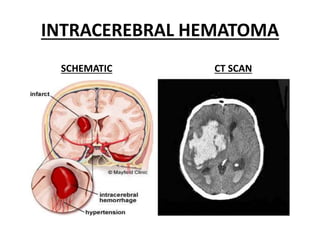
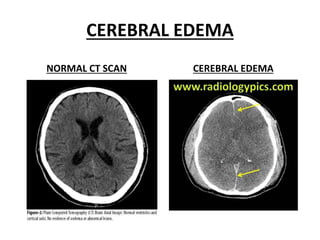
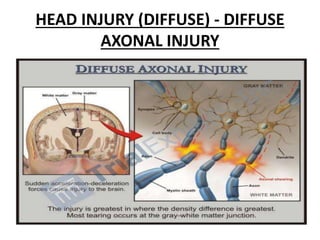
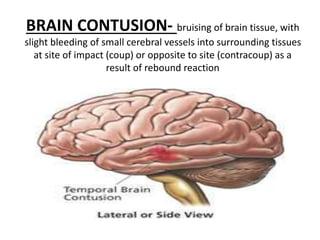
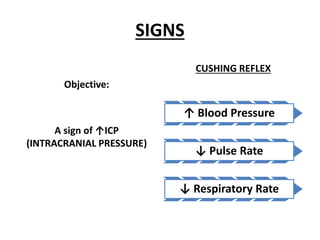
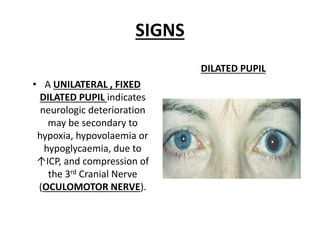
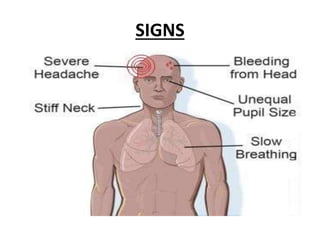
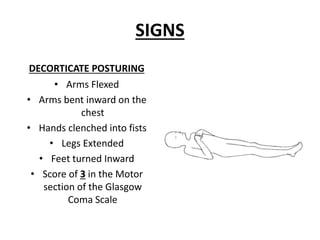
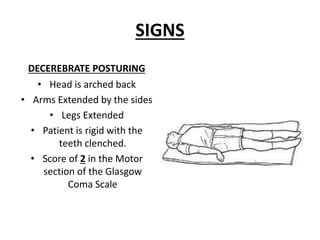
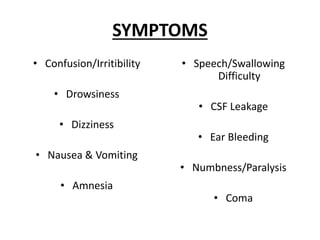
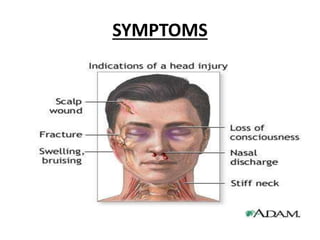
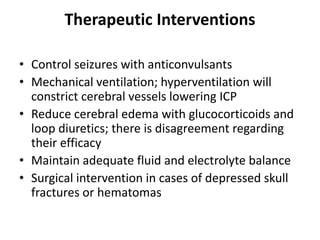
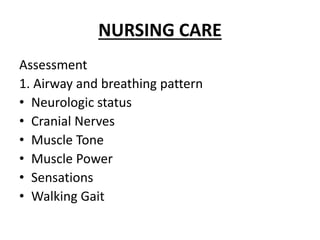
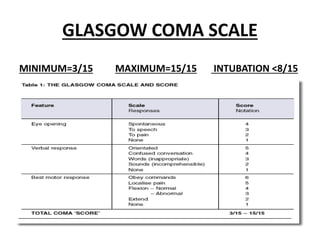
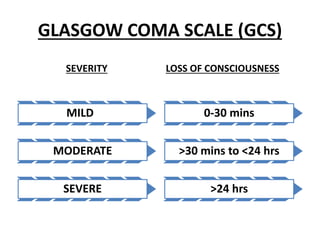
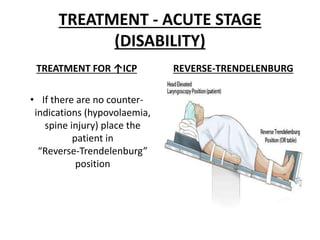
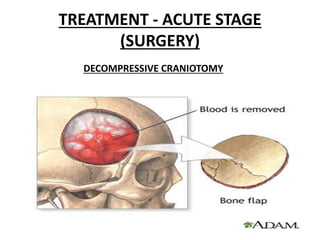
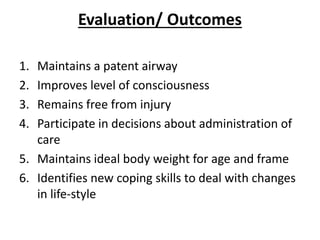
This document defines and describes head injuries and their mechanisms and treatment. It begins by defining head injury and traumatic brain injury. It then describes different types of head injuries like open or closed injuries. It outlines primary and secondary brain injuries and different types of brain hematomas and edema that can occur. The document discusses signs, symptoms, assessments like the Glasgow Coma Scale, treatments like managing increased intracranial pressure, and expected outcomes for patients with head injuries.