This document discusses addiction from several perspectives:
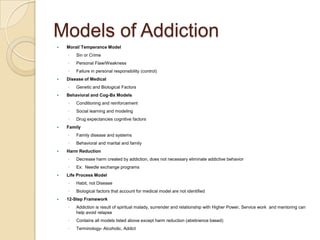
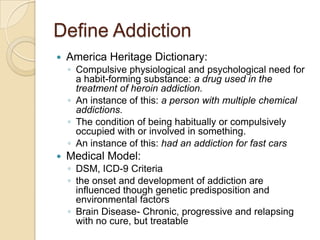
- It defines addiction and outlines several common models of understanding addiction, including moral, disease, behavioral, family systems, harm reduction, and 12-step frameworks.
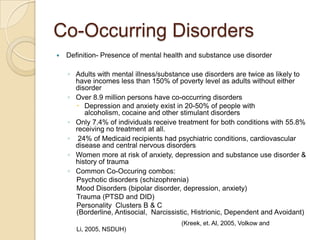
- It reviews common symptoms of addiction like withdrawal and signs of intoxication. Co-occurring disorders are also frequently present.
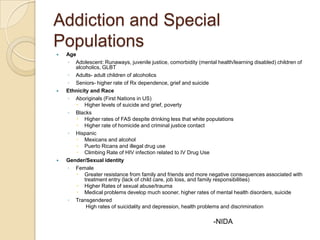
- Special populations like adolescents, ethnic/racial groups, gender identities, and occupational groups may face unique risks and challenges with addiction.
- Implications for practice include controversies in treatment approaches, cultural competence, identification of risk factors, and dual relationship concerns for those in recovery.