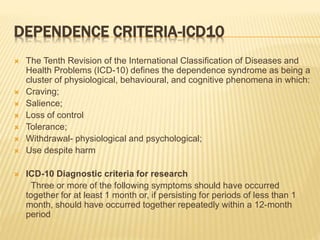
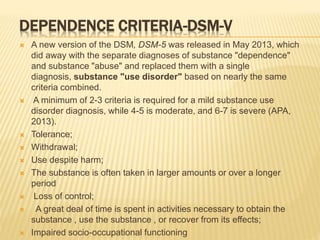
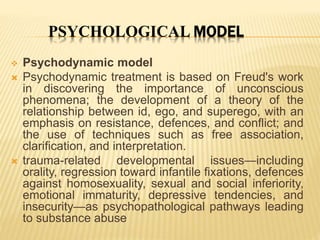
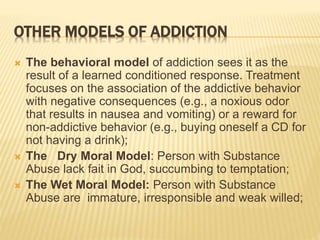
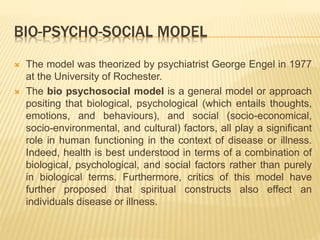
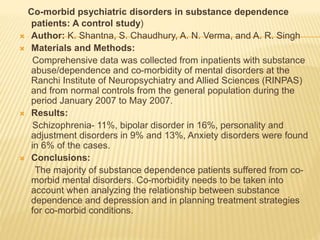
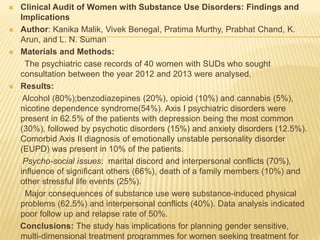
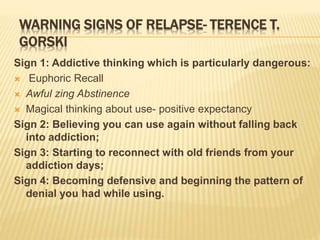
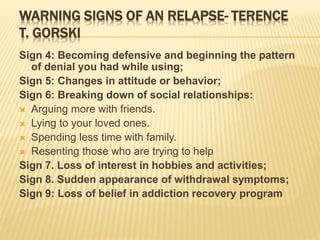
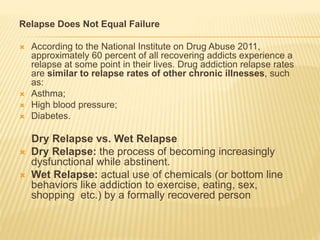
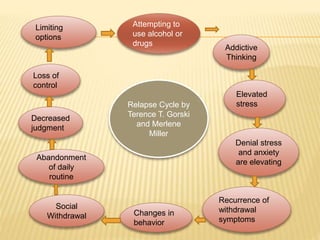
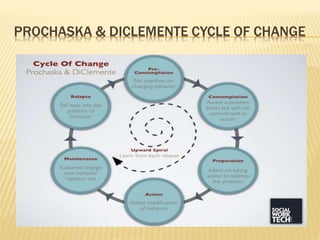
This document outlines relapse prevention strategies presented by Akanksha. It begins with defining dependence and addiction based on ICD-10 and DSM-V criteria. It then discusses various models of addiction including the disease model, psychological models, and the bio-psycho-social model. It also covers the concepts of relapse, warning signs of relapse, and relapse cycles. Finally, it provides an overview of common relapse prevention strategies such as psychoeducation, identifying high-risk situations, developing coping skills and new lifestyle behaviors, increasing self-efficacy, dealing with relapse, and monitoring drug and alcohol use. Family-based approaches to relapse prevention are also briefly discussed.