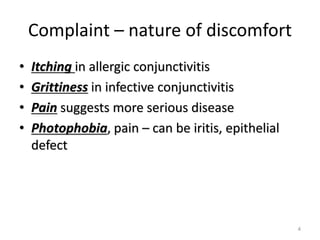
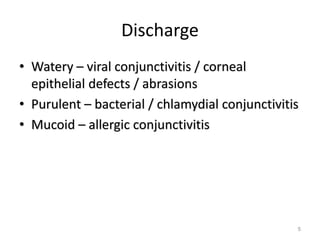
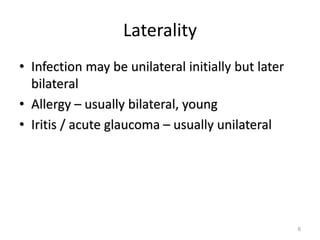
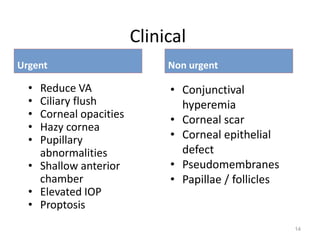
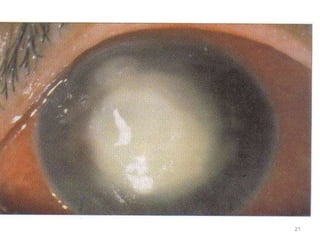
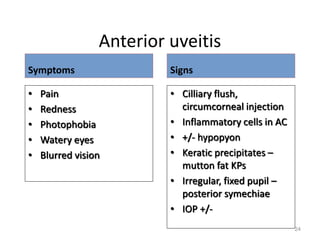
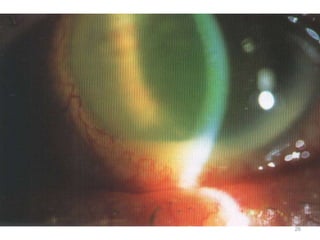
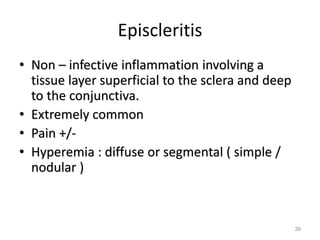
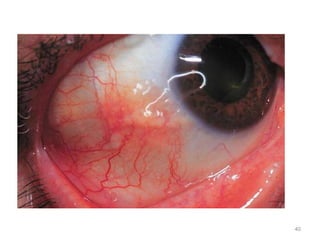
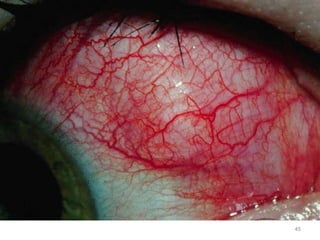
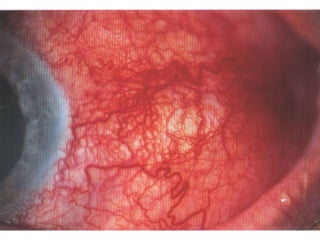
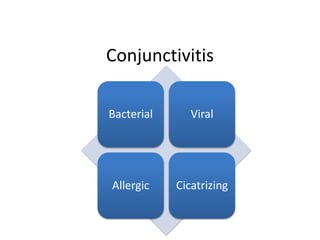
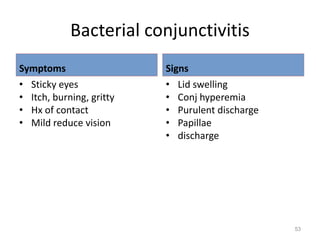
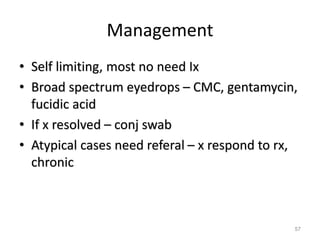
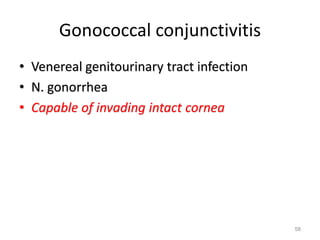
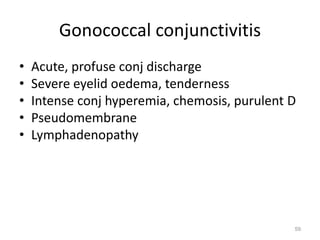
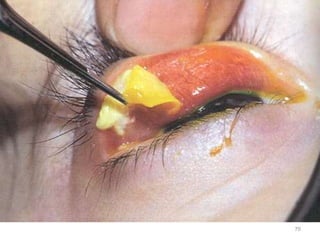
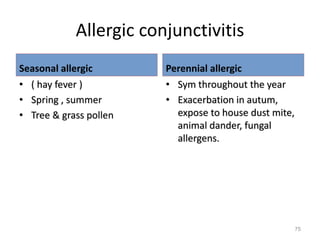
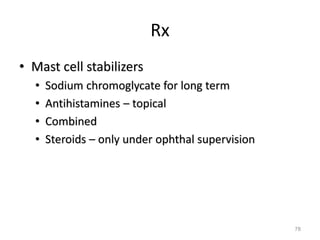
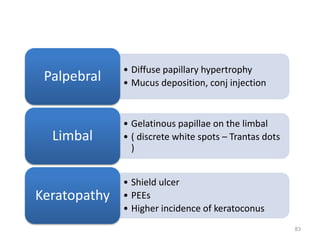
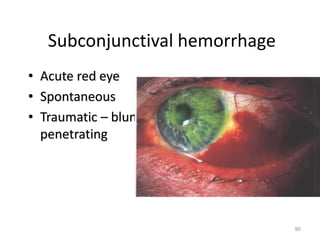
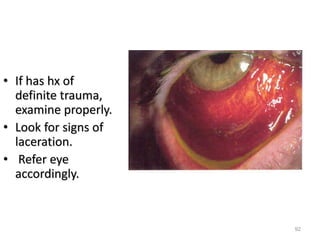
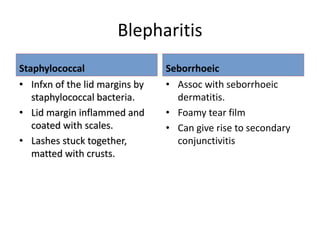
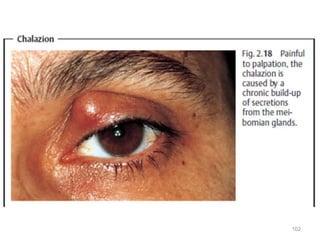
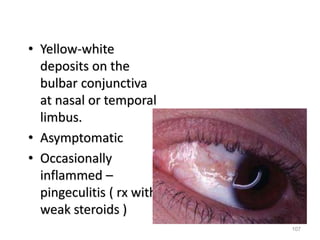
This document provides information on evaluating and differentiating between urgent and non-urgent cases of red eye. It discusses various conditions that can cause red eye including infectious causes like bacterial and viral conjunctivitis, as well as non-infectious causes like allergic conjunctivitis. Clinical features, differential diagnoses, management strategies are outlined for conditions like anterior uveitis, episcleritis, scleritis, blepharitis and subconjunctival hemorrhage. The document emphasizes the importance of identifying vision-threatening conditions like corneal ulcers that require urgent referral and treatment.