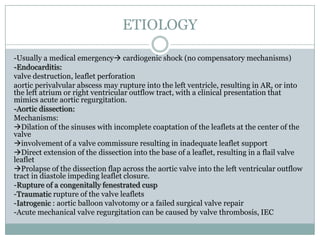
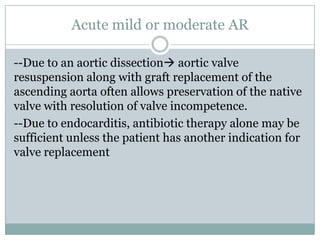
1. Acute aortic regurgitation is a medical emergency that can result from conditions like infective endocarditis, aortic dissection, or trauma.
2. It leads to a sudden rise in left ventricular diastolic pressure and fall in cardiac output, often causing profound hypotension and cardiogenic shock.
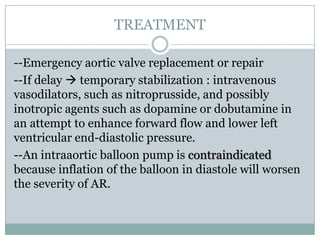
3. Emergency aortic valve replacement or repair is usually required for severe acute aortic regurgitation, while temporary stabilization measures may be used if surgery faces delay.