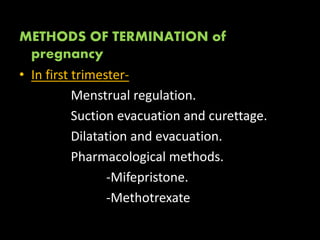
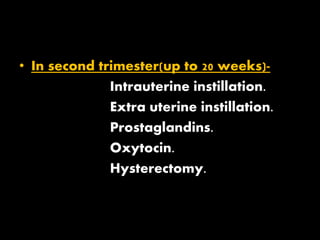
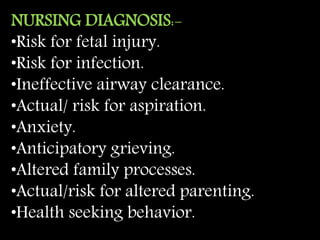
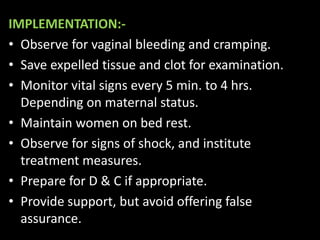
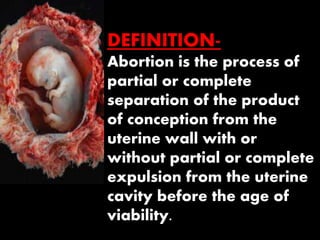
This document defines various types of abortion and provides details about their management. It discusses spontaneous abortions including threatened abortion, inevitable abortion, incomplete abortion, complete abortion, missed abortion, and septic abortion. It also covers induced/electoral abortions, which may be legal under the MTP Act or illegal. Nursing responsibilities are outlined for assessing, planning, implementing, and evaluating care for patients experiencing different types of abortions.



























![MTP [LEGAL ABORTION]
• Since legislation of abortion in India,
deliberate induction of abortion prior to
20 weeks gestation by a registered
medical practitioner in the interest of
mother’s health and life is protected
under the MTP Act.](https://image.slidesharecdn.com/abortionpt-181022042301/85/Abortion-pt-38-320.jpg)