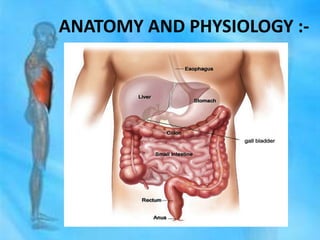
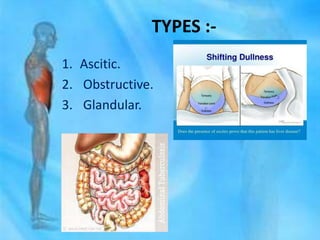
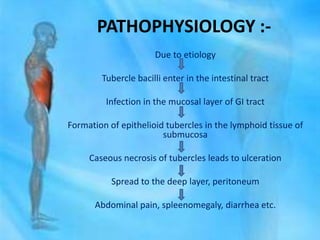
Abdominal tuberculosis is an extra-pulmonary form of tuberculosis affecting the gastrointestinal system, particularly the peritoneum and abdominal lymph nodes. It presents with various symptoms such as abdominal pain, diarrhea, and weight loss, and is diagnosed through tests like biopsies and radiographs. Treatment includes a combination of drug regimens and may involve surgical management, alongside nursing interventions to address pain and nutritional deficits.