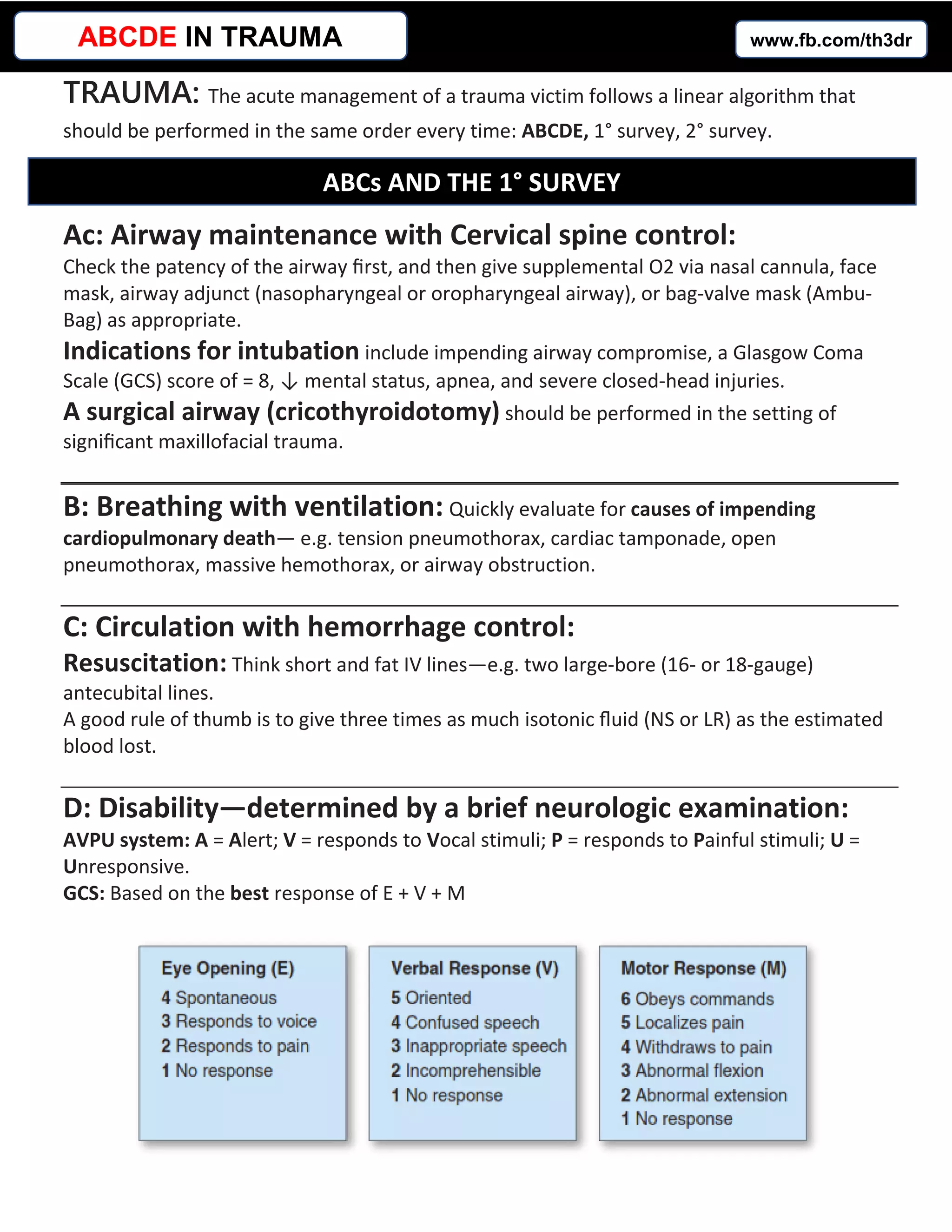
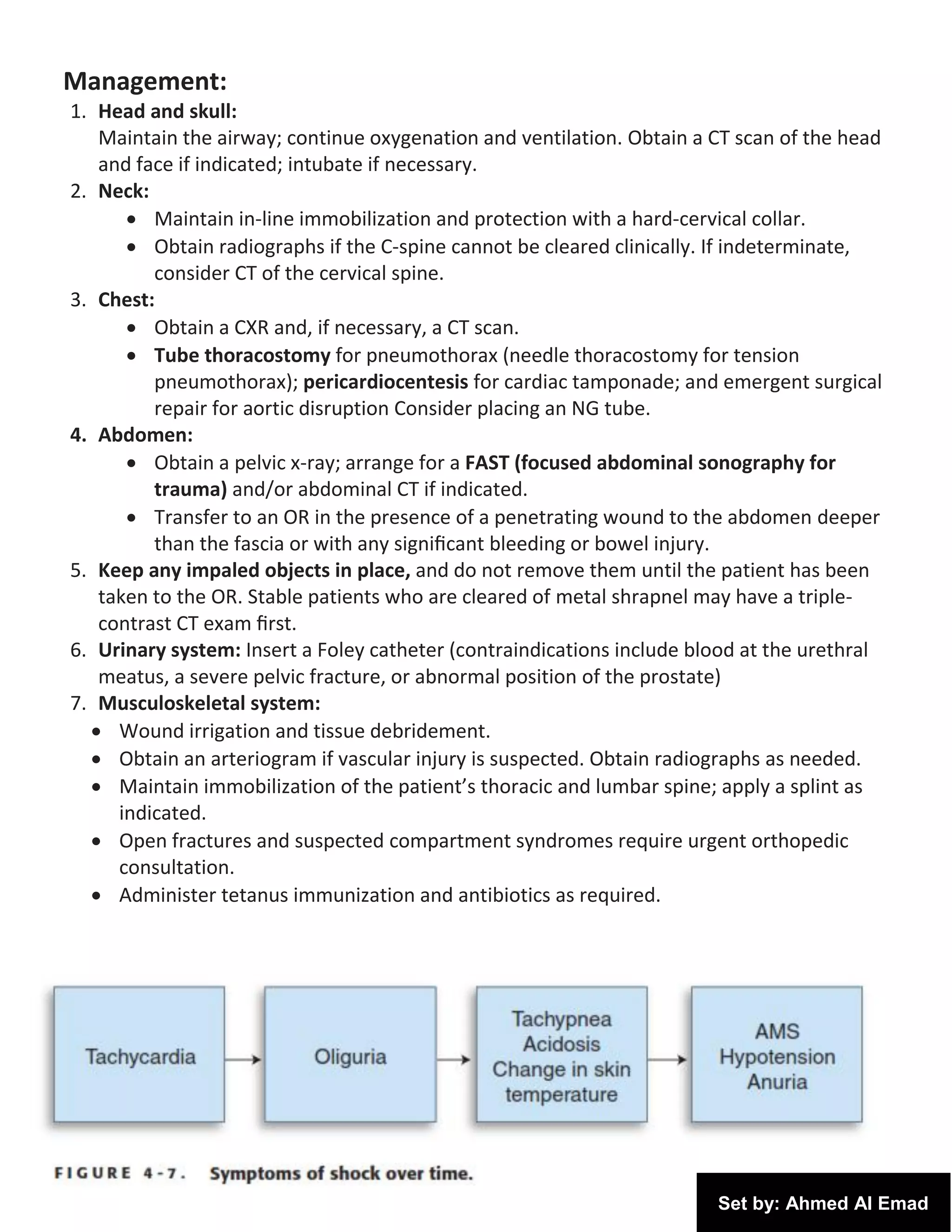
This document outlines the steps for managing a trauma patient according to the ABCDE approach and conducting primary and secondary surveys. The ABCDE approach involves assessing the patient's airway, breathing, circulation, disability, and exposure. The primary survey involves a rapid head-to-toe exam to identify life-threatening injuries. The secondary survey involves a more thorough exam and ordering tests to diagnose and treat injuries found.