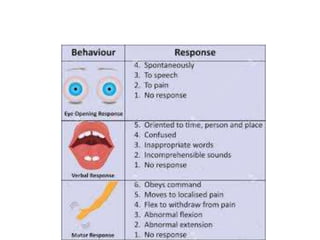
The document discusses the importance of performing a thorough secondary survey on trauma patients to identify injuries that may have been missed in the initial primary survey. It outlines the steps of the secondary survey including obtaining history, examining the head/face, neck, chest, abdomen, extremities, pelvis, neurologic status, and skin. The goal is to identify any injuries that require treatment to prevent morbidity and mortality that could result from delayed diagnosis.