The patient is a 66-year-old African American female presenting with a productive cough and wheezing exacerbated by a panic attack. She has a history of COPD, MAI infection, and other chronic conditions. Diagnostic tests show emphysema and cavities in her lungs. Her MAI infection is likely due to her COPD and she is being treated according to guidelines with a multi-drug regimen to cure her infection and prevent future recurrence of symptoms.

![Patient Case: Subjective
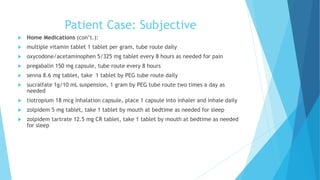
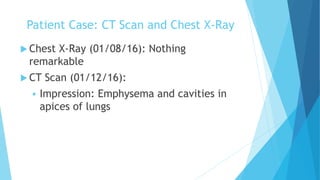
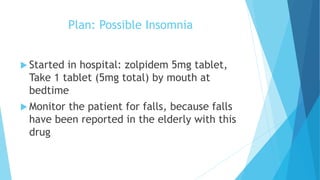
PMH: COPD and emphysema (O2 dependent), MAI infection,
Chronic Sinusitis, former smoker for 35 years (quit 01/01/02),
HTN, LV diastolic dysfunction on post echo, Diabetes with
gastropathy and neuropathy, anemia (chronic, normocytic),
thrombocytopenia, chronic pain (with chronic narcotic therapy
and dependence), chronic low back and abdominal pain,
osteoarthritis with spinal disc disease, former alcohol abuser (quit
in 1993), GERD and esophagitis, esophageal dysmotility and
spasms, odynophagia, dysphagia, PEG tube in place, anxiety and
panic attacks, depression, glaucoma
Past Surgical History: Bronchoscopy 2012; PEG tube placed 2013;
Multiple upper endoscopies and esophageal dilation, plus
manometry; multiple steroid injection, and facet injection as
recently as January 5th [2016].](https://image.slidesharecdn.com/22186829-b613-45fb-b8c4-744650cfed13-161226073017/85/Case-Presentation-MAI-4-320.jpg)
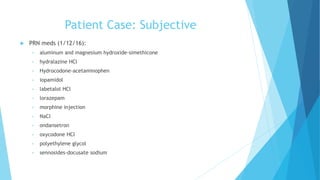



![Clinical Trial: “Efficacy of Clarithromycin and
Ethambutol for Mycobacterium avium Complex
Pulmonary Disease”
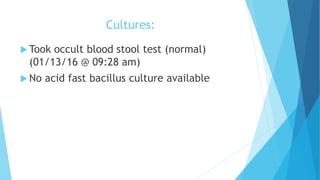
Background: The study assessed the treatment and clinical outcomes of
fibrocavitory pulmonary infection due to Mycobacterium avium complex and
Mycobacterium malmoense with clarithromycin, rifampicin, and ethambutol likely
compared to statistics of those who received rifampicin, ethambutol, with or
without isoniazid.
Methods: Patients who came into the clinic (Royal Infirmary of Edinburgh) from
2001-2007 were given a three-drug regimen. Patients who were immunosuppressed
(HIV, receiving immunosuppressive therapy, cystic fibrosis, DM); 28 total patients
included in the study; were treated with once daily rifampicin (450 mg for
patients who were >50 kg or 600 mg for patients who were >50 kg), once daily
ethambutol (15 mg/kg), and twice daily clarithromycin (500 mg) for 24 months; 14
of the patients had M. avium complex
Statistical Analysis: SPSS, Analysis of Variance with Bonferroni correction for
multiple comparisons, Wilcoxon Test analysis compared 2 treatment time points
Murray MP, Laurenson IF, and Hill AT. Outcomes of a Standardized Triple-Drug Regimen for the Treatment of Nontuberculous Mycobacterial Pulmonary
Infection. Oxford Journals: Clin Infect Dis [Internet]. 2008 July [cited 2016 Feb 23]; 47(2): 222-224. Available from:
http://cid.oxfordjournals.org/content/47/2/222.full.pdf+html .](https://image.slidesharecdn.com/22186829-b613-45fb-b8c4-744650cfed13-161226073017/85/Case-Presentation-MAI-28-320.jpg)
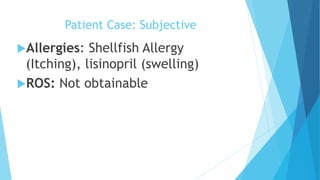
![Clinical Trial: “Efficacy of Clarithromycin and
Ethambutol for Mycobacterium avium
Complex Pulmonary Disease”
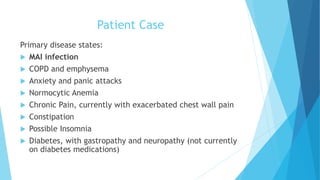
Results: Sputum cultures were positive in one patient at month 6, 2 patients
at month 12, 1 patient at month 18, and 0 patients at months 24 and 30. (Met
P value<0.001)
Recommendations: The three drug recommendation of clarithromycin,
rifampicin, and ethambutol has better efficacy in M. avium complex over a
24 month period compared to those who take rifampicin and ethambutol with
or without isoniazid.
Strengths/Limitations: Strengths: Patients were followed up every 6 months
until 6 months after treatment completion; Patients were followed for at
least 2 years; Data was pulled from patients over a 7 year period (changes in
resistance) Limitations: The trial had only 28 participants and of those only
half of the participants had MAC.
Murray MP, Laurenson IF, and Hill AT. Outcomes of a Standardized Triple-Drug Regimen for the Treatment of Nontuberculous Mycobacterial Pulmonary Infection. Oxford
Journals: Clin Infect Dis [Internet]. 2008 July [cited 2016 Feb 23]; 47(2): 222-224. Available from: http://cid.oxfordjournals.org/content/47/2/222.full.pdf+html .](https://image.slidesharecdn.com/22186829-b613-45fb-b8c4-744650cfed13-161226073017/85/Case-Presentation-MAI-29-320.jpg)

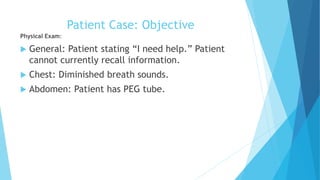
![References
Primary Literature Sources for Main Problem (MAI):
Murray MP, Laurenson IF, and Hill AT. Outcomes of a Standardized Triple-Drug
Regimen for the Treatment of Nontuberculous Mycobacterial Pulmonary Infection.
Oxford Journals: Clin Infect Dis [Internet]. 2008 July [cited 2016 Feb 23]; 47(2):
222-224. Available from:
http://cid.oxfordjournals.org/content/47/2/222.full.pdf+html .
Guidelines for Main Problem (MAI):
Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland
SM, Horsburgh R, Huitt G, Lademarco MF, Iseman M, Olivier K, Ruoss S, Reyn CF,
Wallace Jr. RJ, and Winthrop K, and Mycobacterial Diseases Subcommittee. An
official ATS/IDSA statement: diagnosis, treatment, and prevention of
nontuberculous mycobacterial diseases. Am J of Respir and Crit Care Med
[Internet]. 2007 Jan [cited 2016 Feb 22]; 175(4): 367-416. Available from:
http://www.atsjournals.org/doi/pdf/10.1164/rccm.200604-571ST.](https://image.slidesharecdn.com/22186829-b613-45fb-b8c4-744650cfed13-161226073017/85/Case-Presentation-MAI-50-320.jpg)
![ReferencesOthers:
2014 CHEST Guidelines, Gold Guidelines
2014 AGA Guidelines for IBS
Facts and Comparisons Eanswers. [Internet]. (Netherlands) Alphen aan den Rijn. Wolters Kluwer. [modified 2016; cited 2016 Feb 22].
Available from: http://online.factsandcomparisons.com/index.aspx .
2014 ACCP/CTS Guideline on Prevention of Acute Exacerbations of COPD
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of chronic obstructive
pulmonary disease. Updated 2013. Global Initiative for Chronic Obstructive Lung Disease website.
http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf. Accessed 01/24/16
Reilly, John J., Jr., et al. "Chronic Obstructive Pulmonary Disease." Harrison's Principles of Internal Medicine, 19e. Eds. Dennis Kasper, et
al. New York, NY: McGraw-Hill, 2015. n. pag. AccessMedicine. Web. 26 Jan.
2016.<http://accessmedicine.mhmedical.com/content.aspx?bookid=1130&Sectionid=79745089>.
Bourdet, Sharya V., and Dennis M. Williams. "Chapter 16. Chronic Obstructive Pulmonary Disease." Pharmacotherapy: A Pathophysiologic
Approach, 9e.Eds. Joseph T. DiPiro, et al. New York, NY: McGraw-Hill, 2014. n. pag.AccessPharmacy. Web. 26 Jan.
2016.<http://accesspharmacy.mhmedical.com/content.aspx?bookid=689&Sectionid=48811464>.
Carroll, Karen C., et al. "Mycobacteria." Jawetz, Melnick, & Adelberg’s Medical Microbiology, 27e. Eds. Karen C. Carroll, et al. New York,
NY: McGraw-Hill, 2015. n. pag. AccessMedicine. Web. 30 Jan. 2016.
<http://accessmedicine.mhmedical.com/content.aspx?bookid=1551&Sectionid=94107776>.
2009 American Pain Society, American Academy of Pain Guidelines, “Guideline for the Use of Opioid Therapy in Chronic Non-Cancer Pain,”
2016 ADA Guidelines
Gumbo, Tawanda. "Chemotherapy of Tuberculosis, Mycobacterium Avium Complex Disease, and Leprosy." Goodman & Gilman's: The
Pharmacological Basis of Therapeutics, 12e. Eds. Laurence L. Brunton, et al. New York, NY: McGraw-Hill, 2011. n. pag. AccessPharmacy.
Web. 10 Feb. 2016. <http://accesspharmacy.mhmedical.com/content.aspx?bookid=1613&Sectionid=102163458>.
Dynamed. DynaMed Plus [Internet]. Ipswich (MA): EBSCO Information Services. 1995 – [cited 2016 Feb 10]. Available from
http://www.www.dynamed.com. Registration and login required.
Lexicomp. Lexidrugs. Hudson, Ohio: 2016. Lexicomp, Inc.; Feb 10, 2016.](https://image.slidesharecdn.com/22186829-b613-45fb-b8c4-744650cfed13-161226073017/85/Case-Presentation-MAI-51-320.jpg)