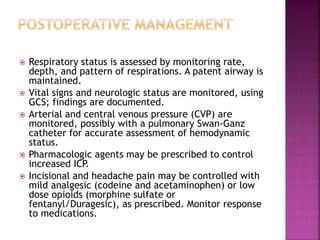
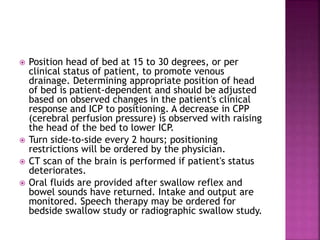
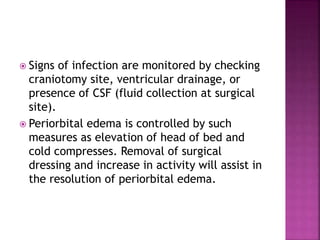
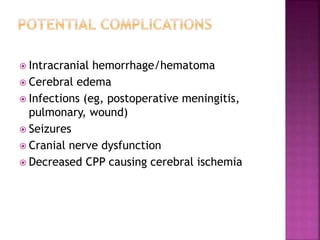
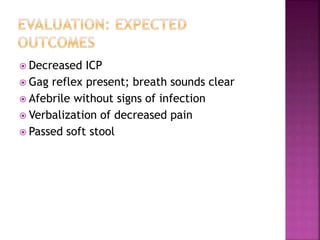
This document outlines postoperative care considerations following craniotomy. It describes monitoring vital signs and neurological status, maintaining normal intracranial pressure, preventing infections and aspiration, managing pain, avoiding constipation, and providing patient and family education. Close observation is needed to monitor for complications like hemorrhage, edema, seizures, and infection.
![ If cerebral edema develops, intraoperative or
postoperative osmotic diuretic (mannitol
[Osmitrol]) or corticosteroids may be ordered for
its treatment.
Neurologic assessment is performed to evaluate
and record the patient's neurologic baseline and
vital signs for postoperative comparison.
Family and patient are made aware of the
immediate postoperative care and where the
physician will contact the family after surgery.
Supportive care is given as needed for neurologic
deficits.](https://image.slidesharecdn.com/5-240213133105-cd8f8e53/85/5-INTRACRANIAL-SURGERY-nursing-processpptx-4-320.jpg)