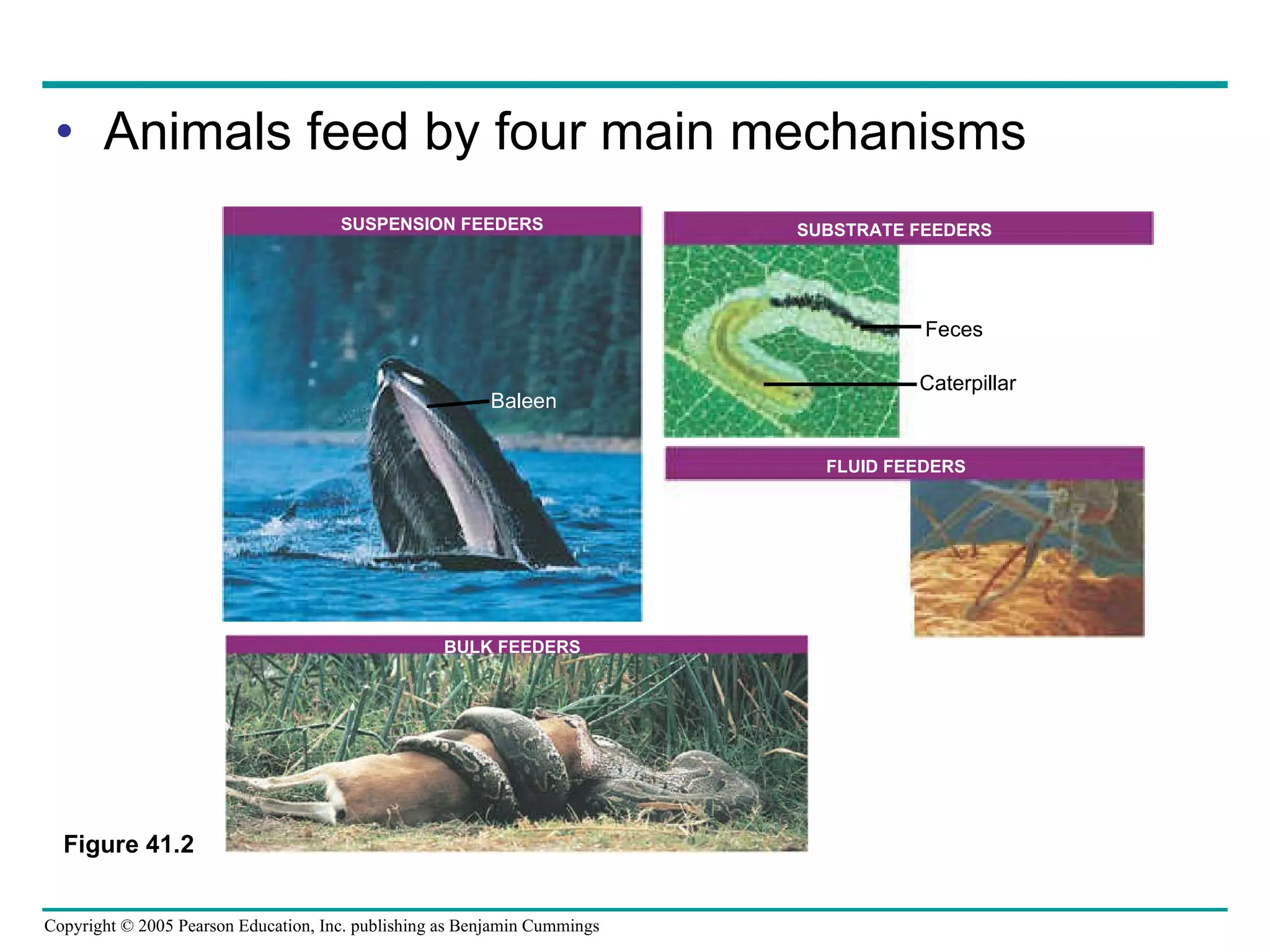
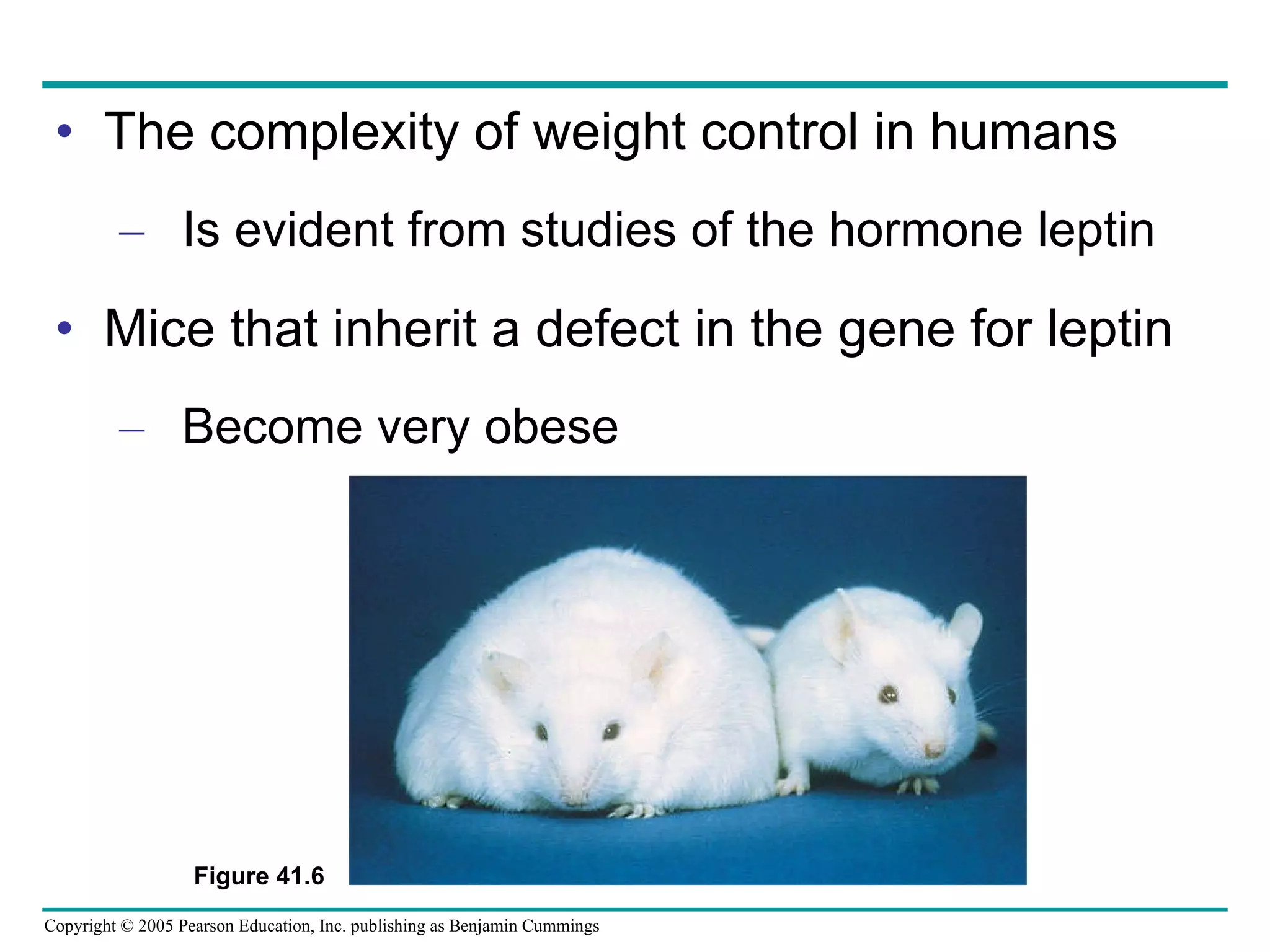
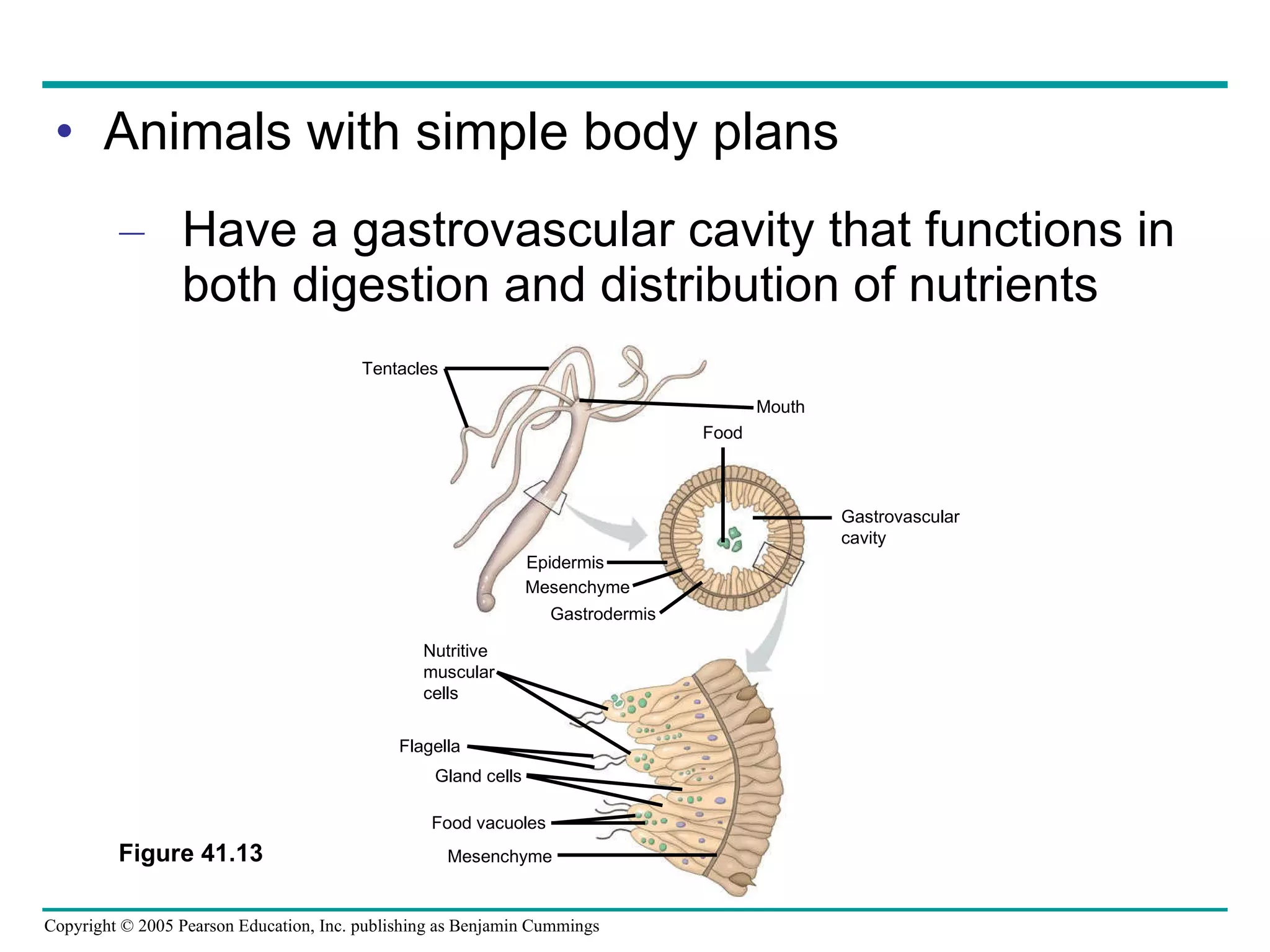
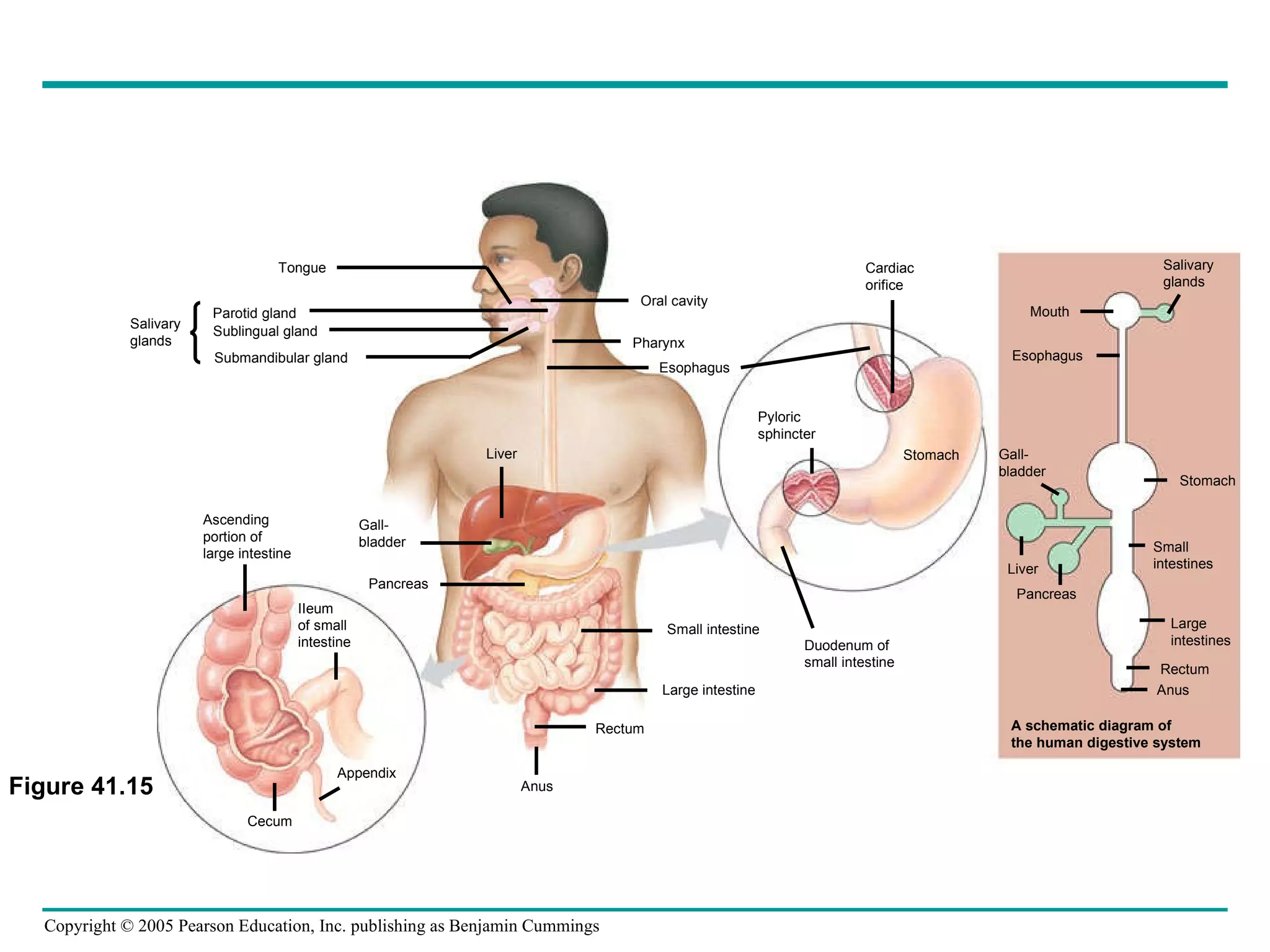
The document provides an overview of animal nutrition and digestion. It discusses that animals fall into three dietary categories - herbivores, carnivores, and omnivores. The main stages of food processing in animals are ingestion, digestion, absorption, and elimination. Digestion occurs through specialized digestive organs and glands that break down food into smaller molecules for absorption. Homeostatic mechanisms regulate nutrient intake and storage to maintain energy balance.