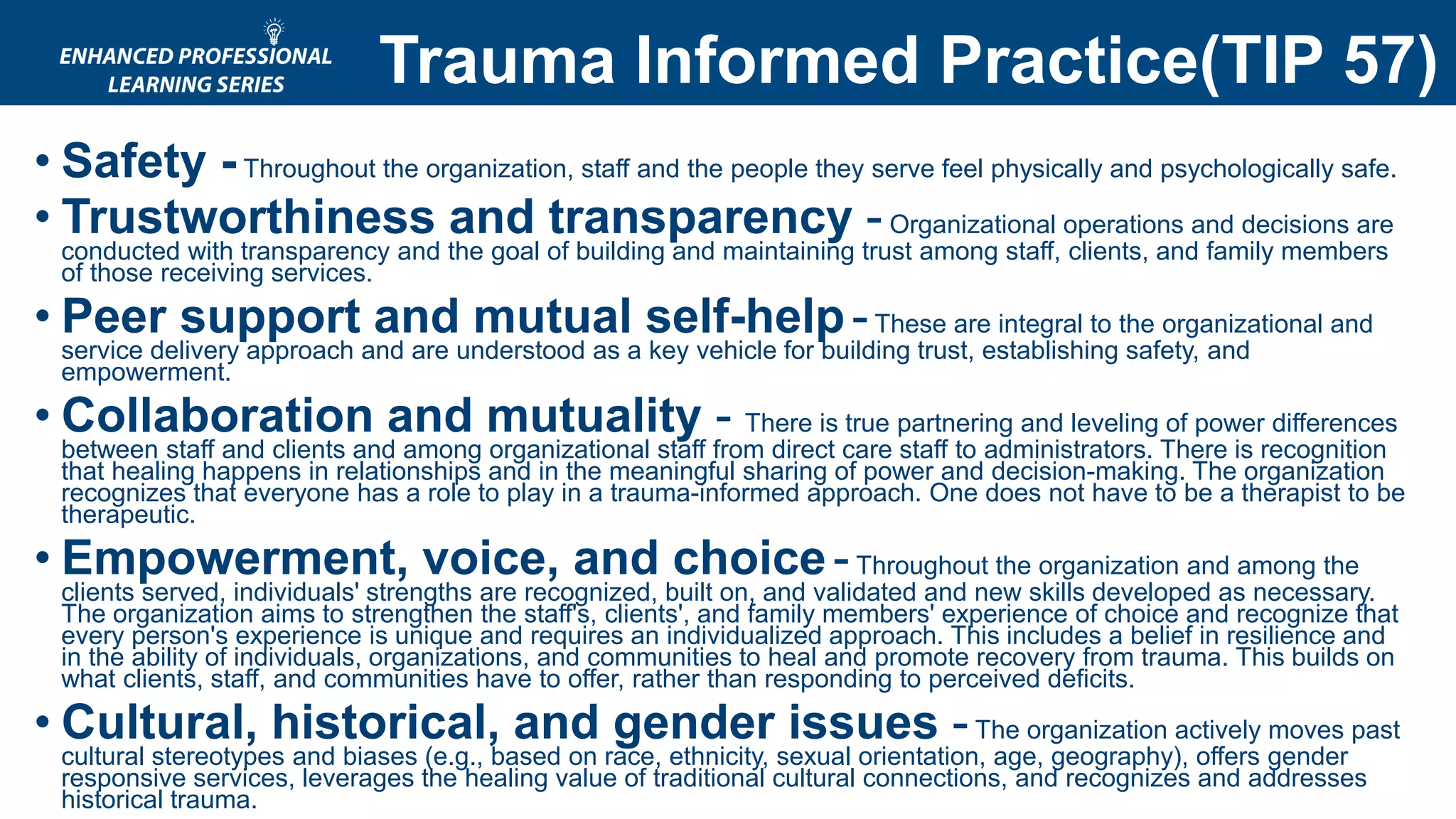
The document provides an agenda for a training session on anxiety, trauma, and stress for practitioners working with clients with co-occurring disorders. The agenda includes: a check-in, a review of a stress video and discussion, a presentation on signs and symptoms of anxiety disorders and how stress relates, a discussion on trauma experienced by clients and practitioners, a preview of the next session, and a question period. The document also includes supplementary materials on anxiety disorders, trauma-informed practices, secondary trauma, and self-care strategies.