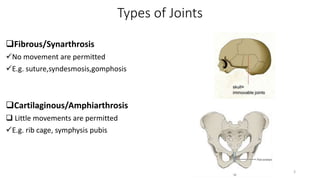
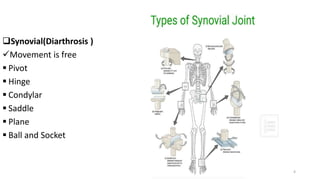
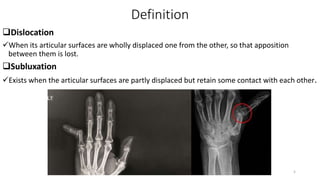
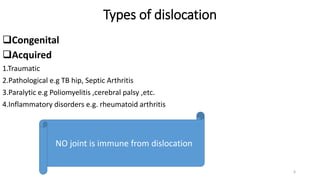
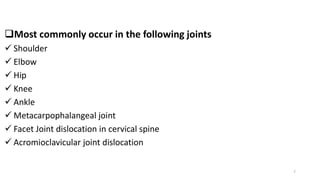
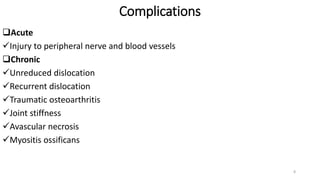
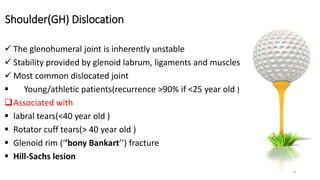
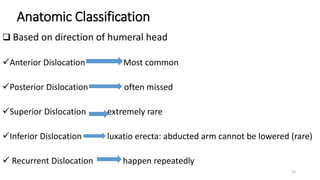
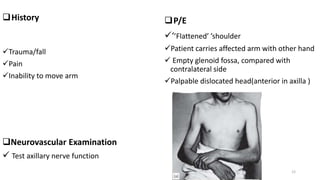
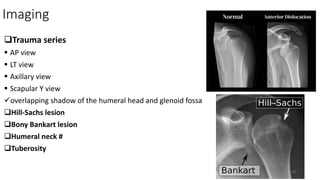
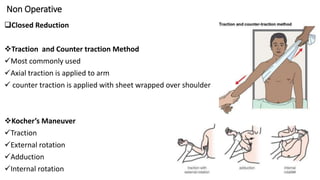
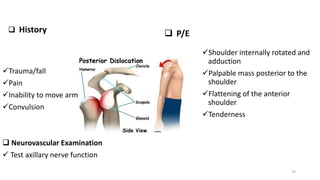
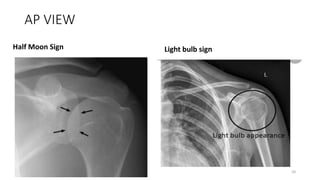
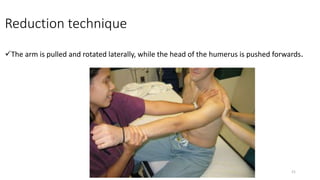
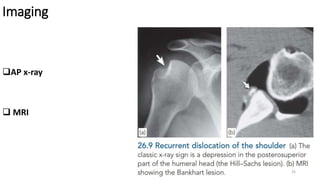
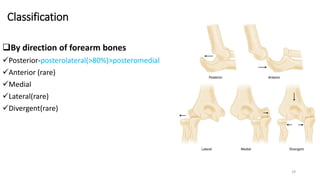
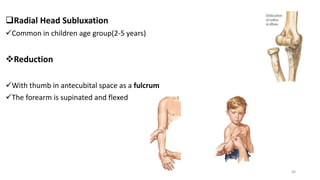
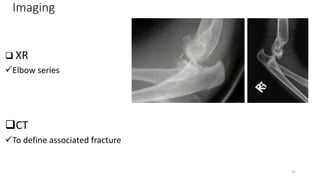
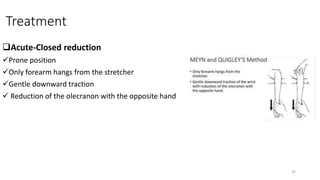
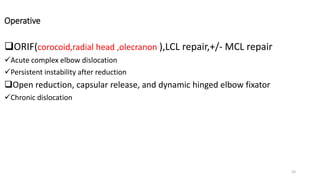
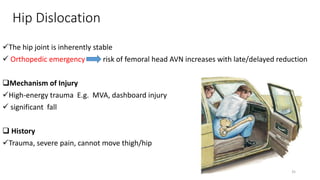
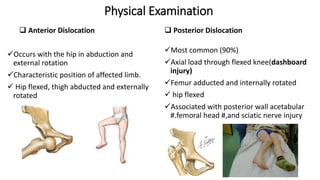
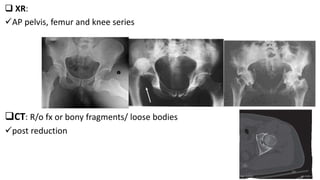
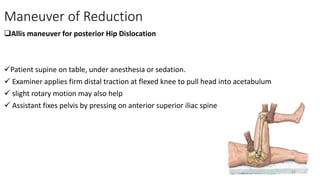
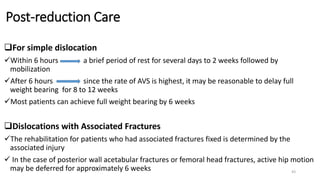
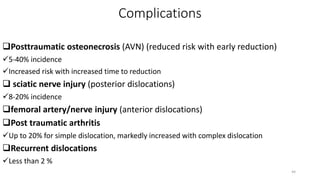
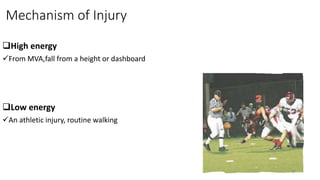
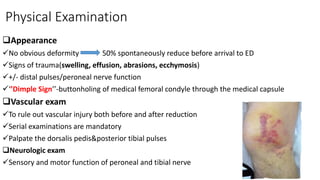
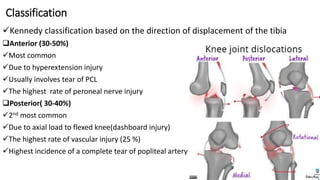
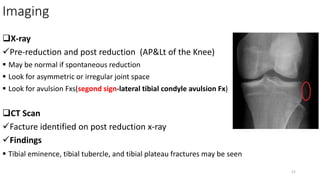
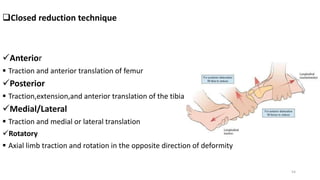
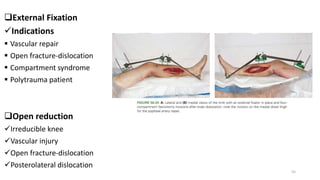
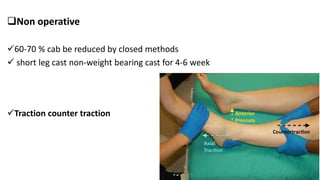
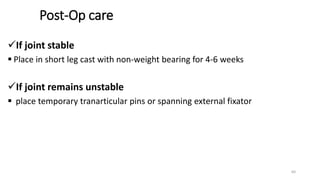
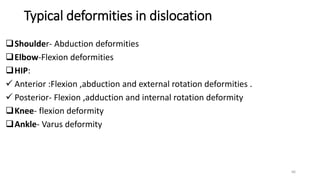
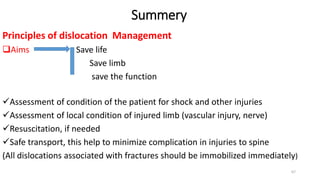
This document outlines principles of managing common joint dislocations. It discusses the anatomy, mechanisms, clinical presentation, imaging and treatment approaches for dislocations of the shoulder, elbow, hip and knee. For each joint, it describes techniques for closed and open reduction as well as post-reduction care and rehabilitation. Complications of joint dislocations like recurrent instability, stiffness and avascular necrosis are also summarized.