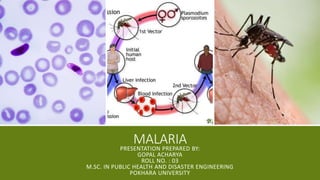
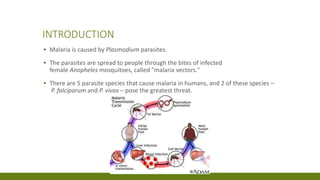
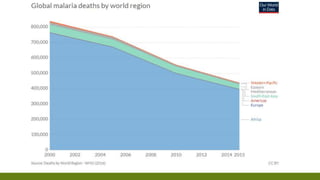
Malaria is caused by Plasmodium parasites transmitted through mosquito bites. It remains a major public health problem, with over 200 million cases and 400,000 deaths annually. Young children and pregnant women are most vulnerable. Prevention focuses on insecticide-treated bed nets, indoor residual spraying, antimalarial drugs, and surveillance. The Global Technical Strategy aims to reduce cases and deaths by 90% by 2030. National initiatives like Roll Back Malaria and High Burden High Impact work to eliminate malaria. Nepal aims to be malaria-free by 2025 through prevention, diagnosis and treatment programs.