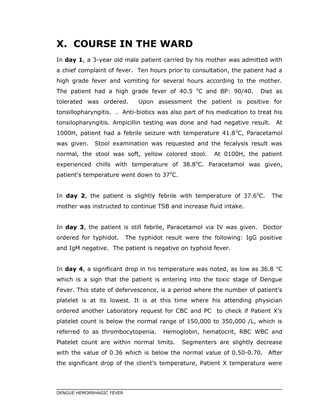
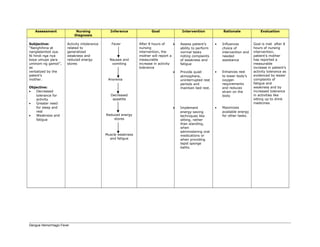
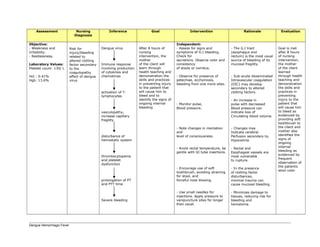
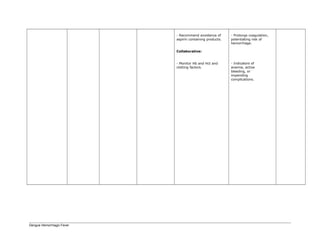
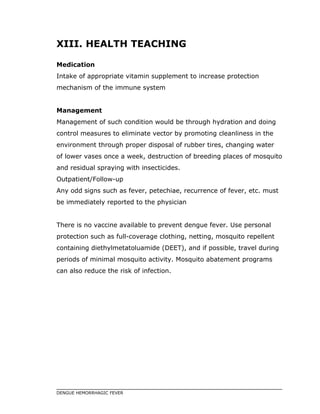
This document is a case study on dengue hemorrhagic fever (DHF) focusing on a 3-year-old male patient diagnosed with DHF category II. It details the patient's clinical symptoms, hospital management, and treatment process over a seven-day stay, highlighting the significance of dengue as a prevalent mosquito-borne disease. The study aims to enhance understanding of DHF through nursing practice while emphasizing the need for awareness and proper management of dengue in healthcare settings.










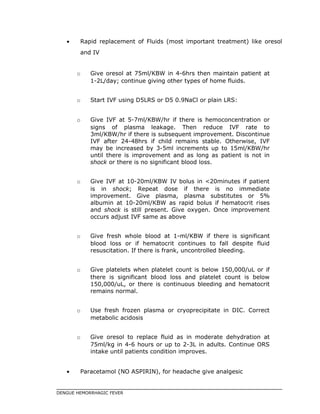
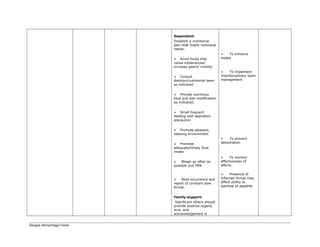
![neutrophils (mature form of a WBC), and 175 billion platelets each day.
When the body needs more blood cells, as in infection (when WBCs are
needed to fight the invading pathogen) or in bleeding (when more RBCs are
required), the marrow increases its production of the cells required. Thus,
under normal conditions, the marrow responds to increased demand and
releases adequate numbers of cells into the circulation.
The volume of blood in humans is approximately 7% to 10% of the normal
body weight and amounts to 5 to 6 L. Circulating through the vascular
system and serving as a link between body organs, the blood carries oxygen
absorbed from the lungs and nutrients absorbed from the gastrointestinal
tract to the body cells for cellular metabolism. Blood also carries waste
products produced by cellular metabolism to the lungs, skin, liver, and
kidneys, where they are transformed and eliminated from the body. Blood
also carries hormones, antibodies, and other substances to their sites of
action or use.
Blood is made up of plasma (fluid component) and formed elements (cellular
component). Plasma consists of about 90% water and 10% solutes
(electrolytes, albumin, globulins, and clotting factors). The formed elements
include erythrocytes (red blood cells
[RBCs]), leukocytes (white blood
cells [WBCs]), and platelets (PLTs).
To function, blood must remain in its
normally fluid state. Because blood
is fluid, the danger always exists
that trauma can lead to loss of blood
from the vascular system. To
prevent this, an intricate clotting
mechanism is activated when
necessary to seal any leak in the
blood vessels. Excessive clotting is
equally dangerous, because it can obstruct blood flow to vital tissues. To
DENGUE HEMORRHAGIC FEVER](https://image.slidesharecdn.com/236750009-dengue-case-study1-150913051028-lva1-app6892/85/236750009-dengue-case-study1-13-320.jpg)