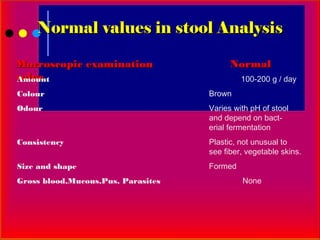
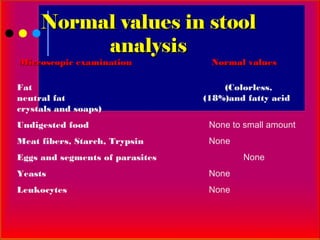
1. The stool or feces consists of undigested food materials, bacteria, epithelial cells, leukocytes, and other components.
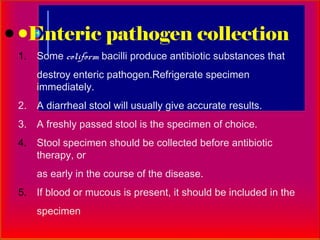
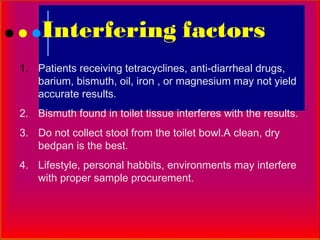
2. For a stool analysis, random stool samples should be collected using universal precautions and delivered immediately without contamination.
3. Multiple stool samples over several days are recommended when checking for parasites due to their life cycles.