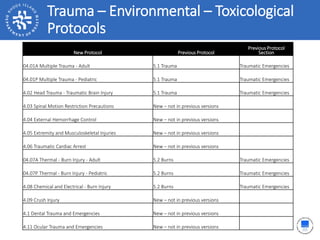
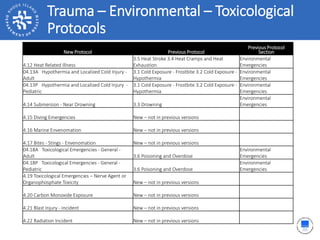
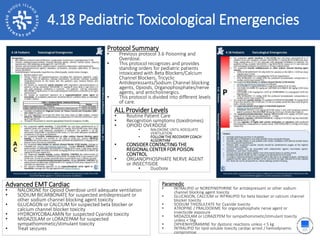
This document outlines new protocols for trauma, environmental, and toxicological emergencies in Rhode Island. It summarizes 24 new protocols which consolidate and replace several previous protocols. The protocols provide guidance for all levels of emergency responders on treatments for injuries such as burns, hypothermia, drowning, and envenomation. They emphasize rapid treatment and transport of critically injured patients.

![2.17 Obstetrical Delivery4.19 Nerve Agent or Organophosphate Toxicity
ALL Provider Levels
• Routine Patient Care
• PPE
• DuoDote
• Adult
• Pediatric
Protocol Summary
• New Protocol
• This protocol recognizes and provides standing orders for patient with suspected or know
exposure to a nerve or organophosphate agent with salivation, lacrimation, urination,
defecation, GI distress, emesis [SLUDGE], muscle twitching, seizures, respiratory arrest),
bradycardia, bronchorrhea, and/or bronchospasm.
• This protocol is divided into different levels of care.
Advanced EMT Cardiac
• Manage Seizures as per the age appropriate Seizure Protocol
Paramedic
• Manage Seizure as per the age appropriate Seizure Protocol
• ATROPINE / PRALIDOXIME for organophosphate nerve agent or insecticide exposure](https://image.slidesharecdn.com/2017ristatewideemsprotocols-educationmodules-section4-161025104339/85/2017-RI-Statewide-EMS-Protocols-Education-Modules-Section-4-30-320.jpg)