The document describes the Emergency Severity Index (ESI), a 5-level triage system used in emergency departments.
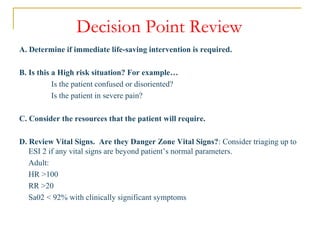
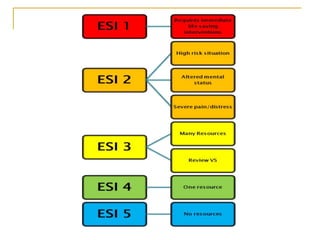
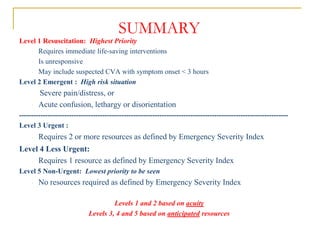
Level 1 is the highest priority and requires immediate life-saving interventions for patients who are unresponsive. Level 2 is also high priority for patients with severe pain/distress or acute confusion.
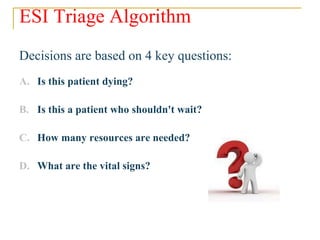
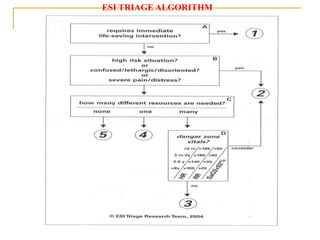
Levels 3, 4, and 5 are determined based on the number of resources (staff and equipment) needed, with Level 3 requiring 2 or more resources, Level 4 requiring 1 resource, and Level 5 requiring no resources. The ESI algorithm uses 4 questions to rapidly sort patients based on acuity and resource needs.
The ESI system aims to get the right patient to the right resources at