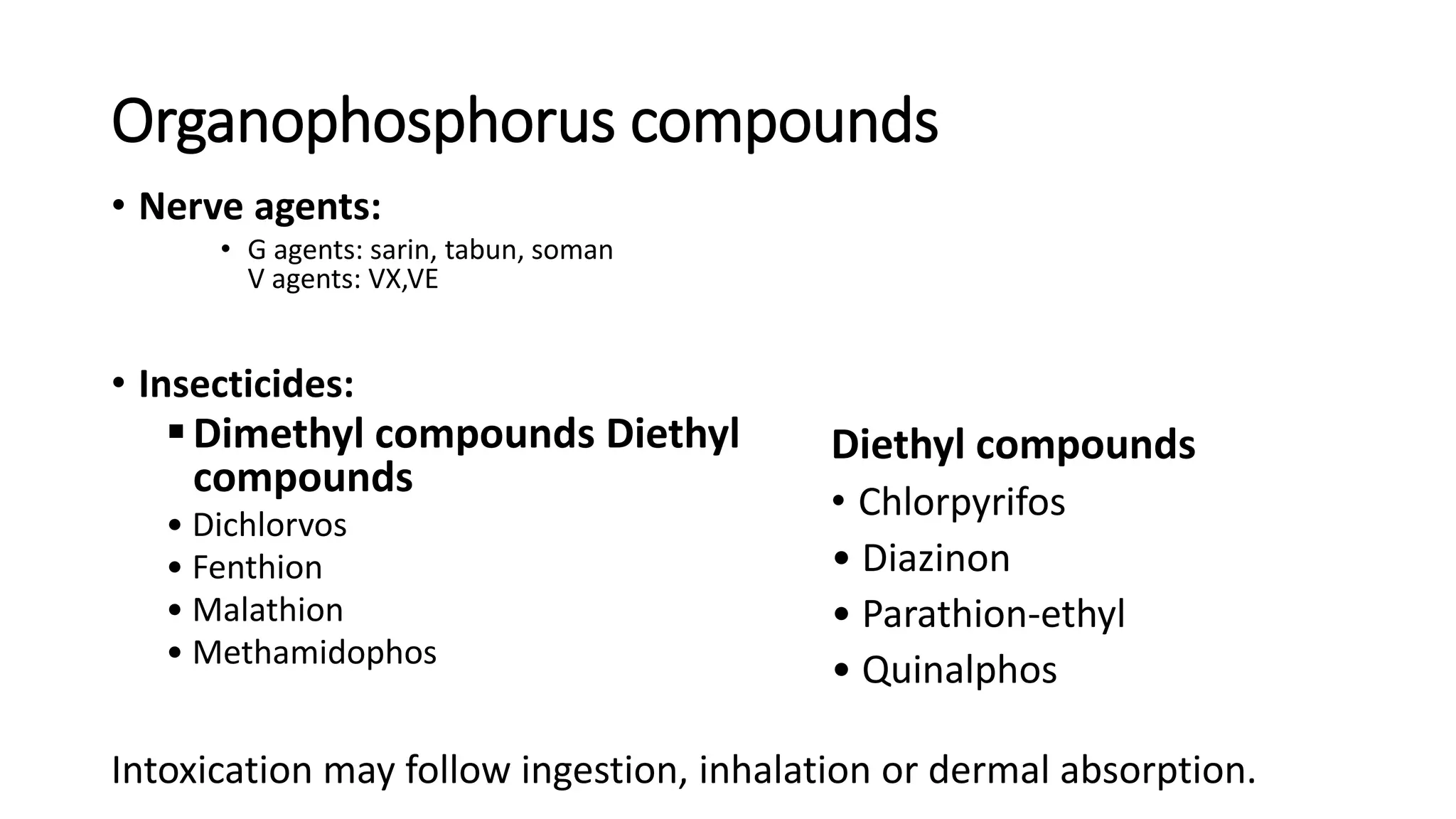
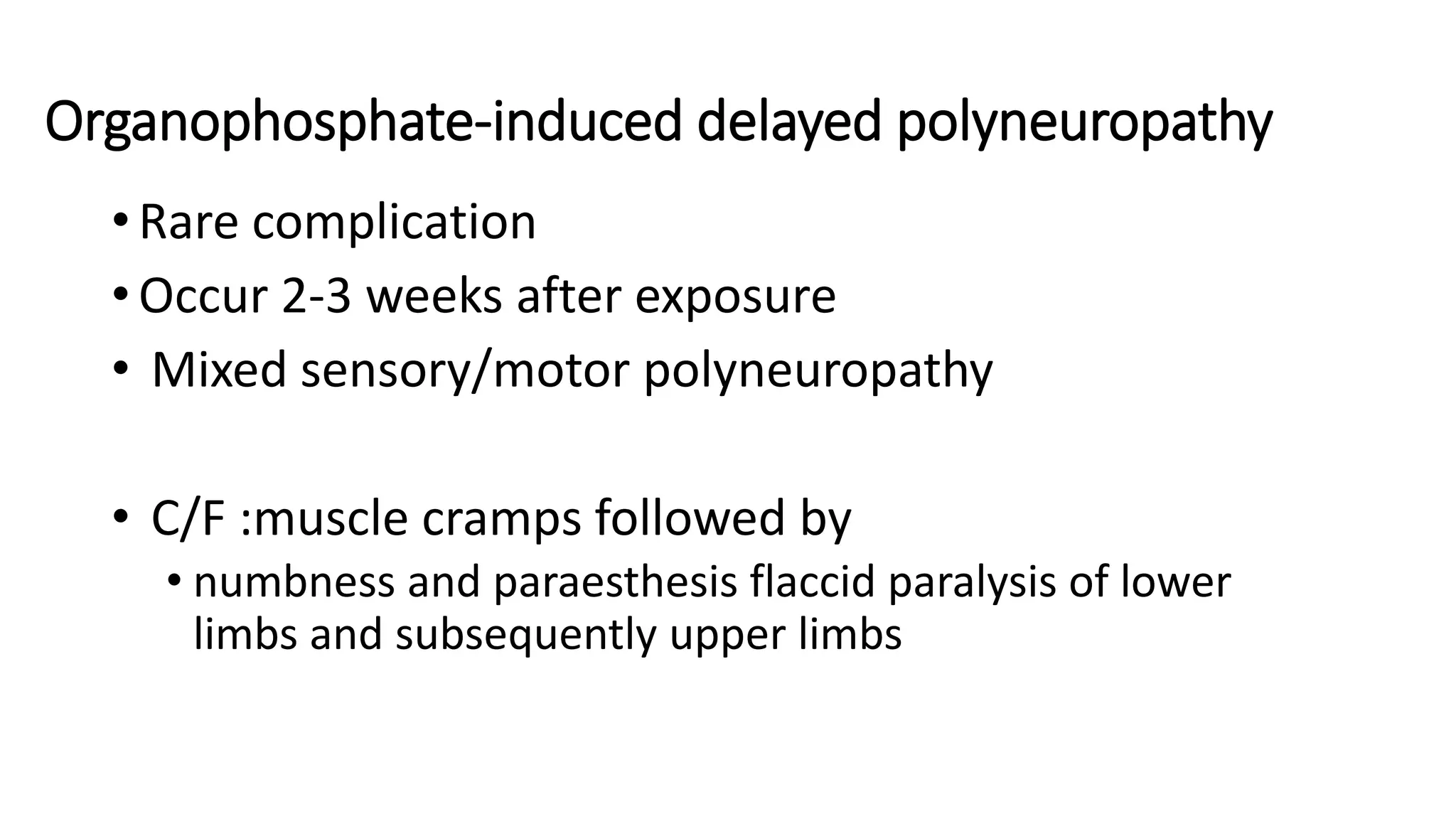
The document discusses organophosphate poisoning, detailing the types of compounds involved, mechanisms of toxicity, and clinical features such as cholinergic symptoms and intermediate syndrome. Management includes supportive care, decontamination, and the use of antidotes like atropine and pralidoxime. It emphasizes the importance of airway maintenance and addresses potential complications following exposure.