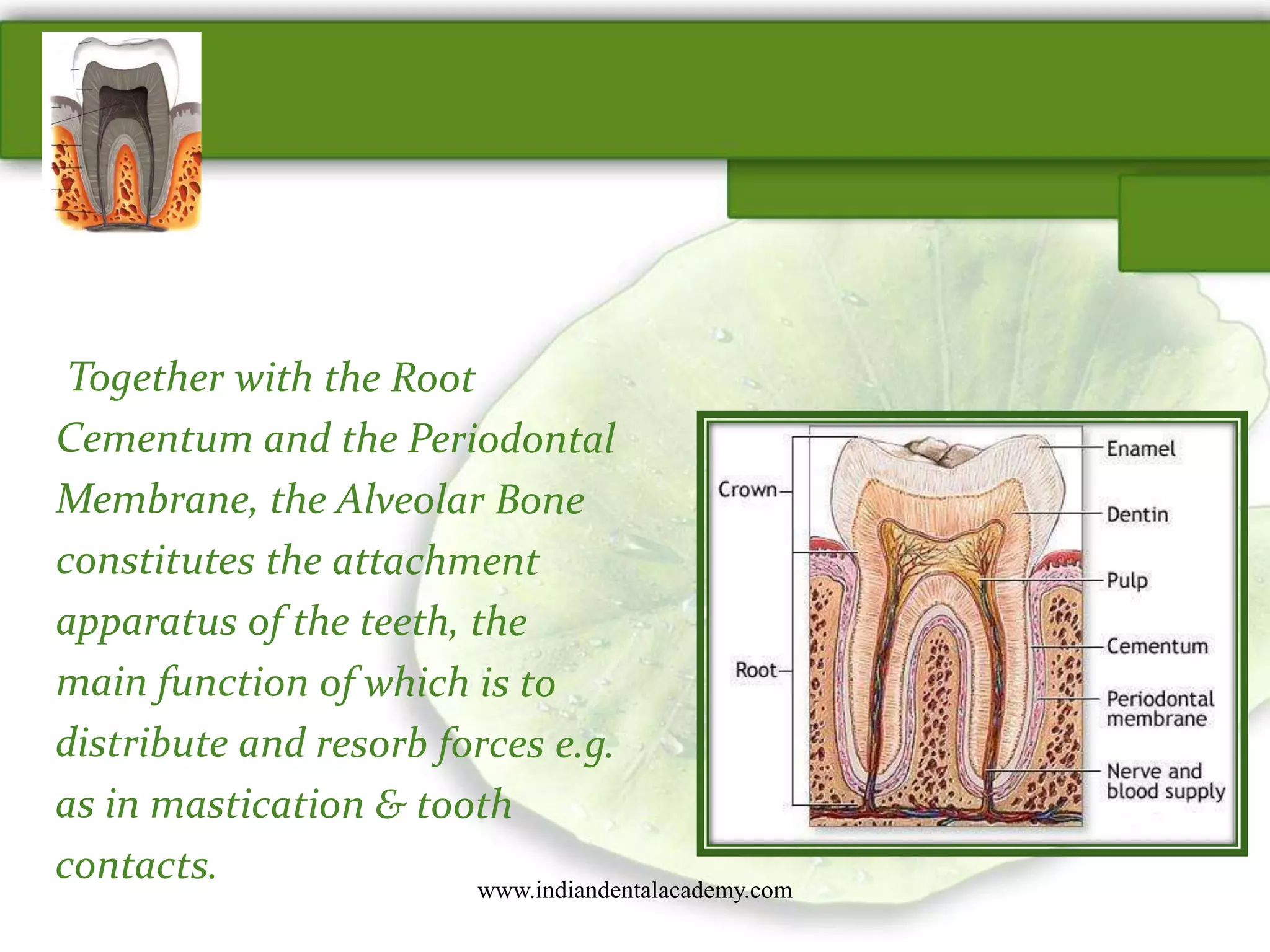
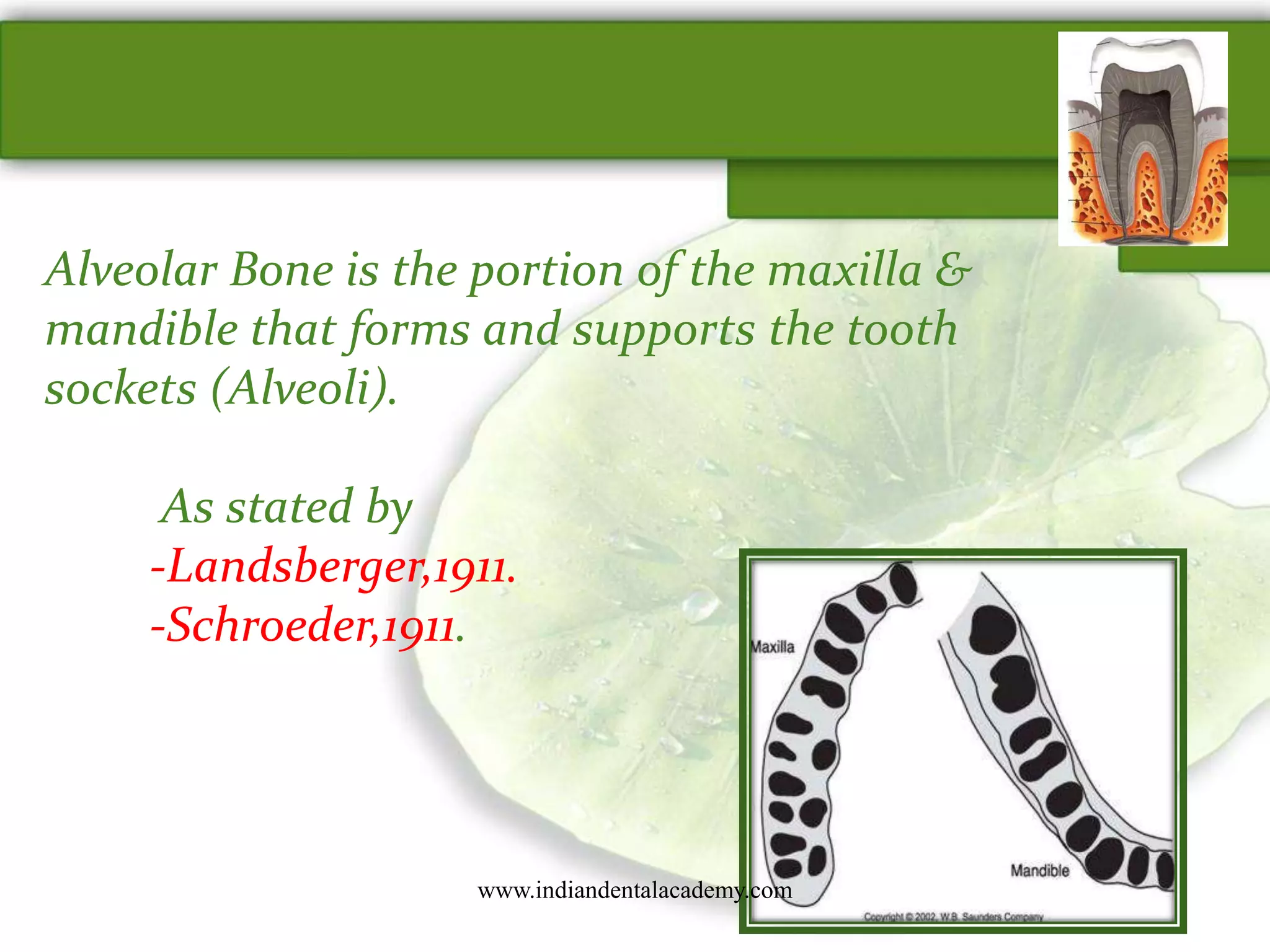
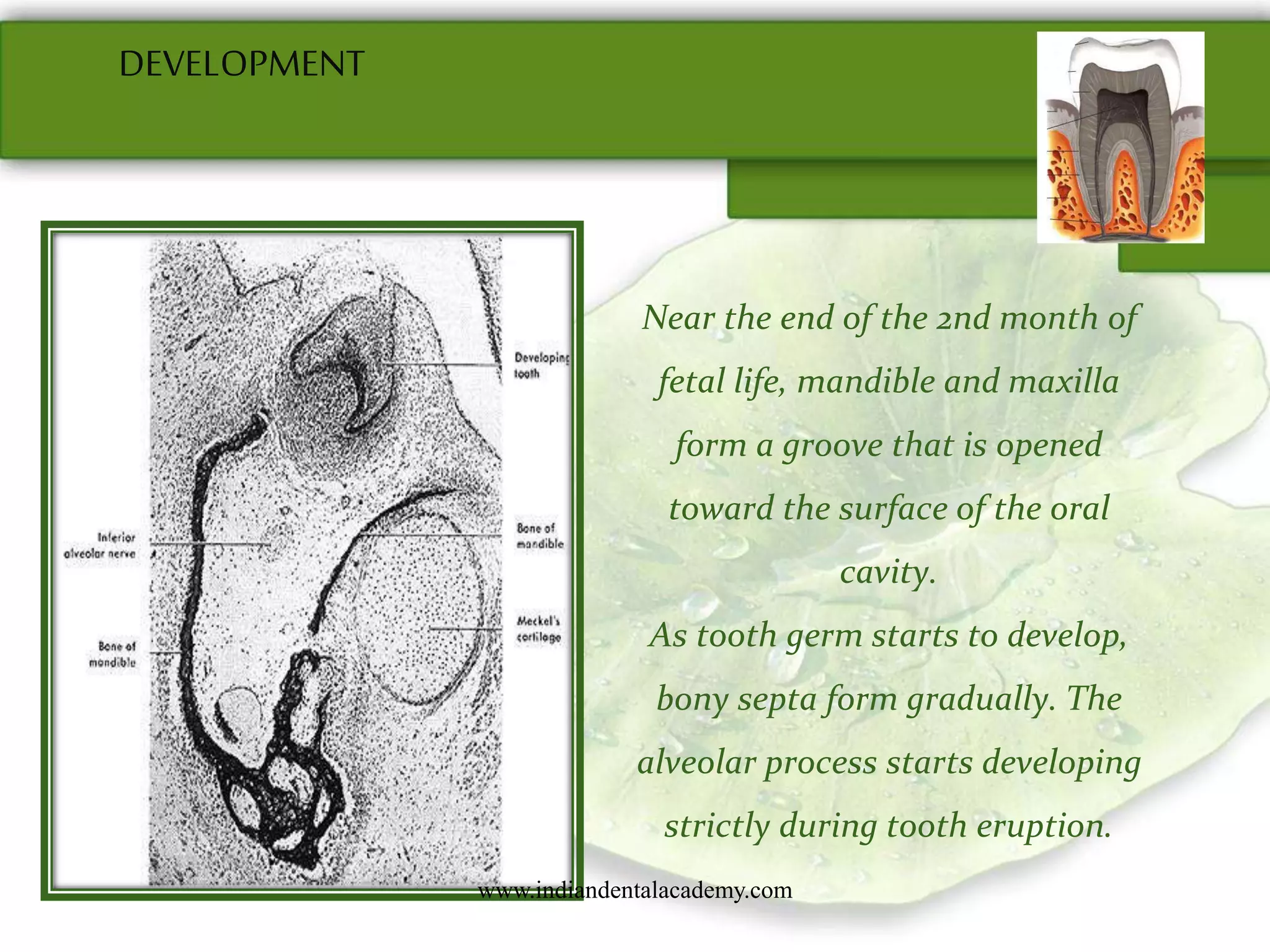
Alveolar bone forms the sockets that hold teeth and is composed of alveolar bone proper surrounding tooth roots and supporting alveolar bone. It develops during tooth eruption through both intramembranous and endochondral ossification. Alveolar bone is maintained through remodeling where bone resorption by osteoclasts is followed by bone formation by osteoblasts, regulated by hormones and growth factors to maintain calcium homeostasis.

















































![Recognition of extra cellular
Bone matrix proteins
Osteoclast polarization [Clear zone, Ruffledborder ]
Martin and Ng 1994 Local factors
Fuller et al1991 Osteoblast
Osteoclast activation
Laotiala1994 H + ions
Hill et al 1993 Proteolyticenzymes
Bone resorption
Arrest of osteoclast activitywww.indiandentalacademy.com](https://image.slidesharecdn.com/1-160428061832/75/alveolar-process-56-2048.jpg)












