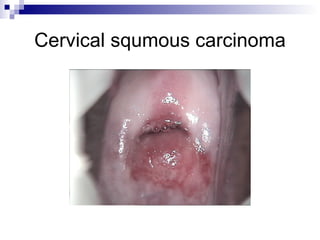
Cervical dysplasia and cervical cancer are caused by HPV infection, with high-risk factors including young age at first intercourse, multiple sexual partners, and smoking. Precancerous lesions are classified as CIN (cervical intraepithelial neoplasia) grades 1-3 based on pathology. Diagnosis involves cytology, colposcopy, and biopsy. Treatment depends on cancer stage and may include surgery, radiation, or chemoradiation.
![Cervical Dysplasia and Cervical Cancer Qu Quanxin [email_address] Tianjin First Central Hospital](https://image.slidesharecdn.com/18-cervicalcancer-090507103853-phpapp02/85/18-Cervical-Cancer-1-320.jpg)