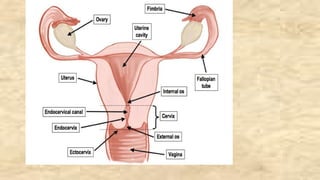
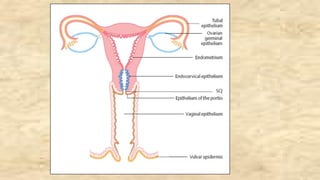
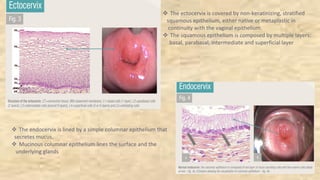
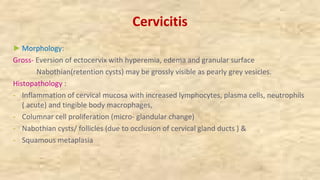
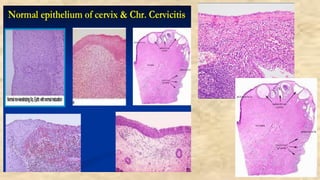
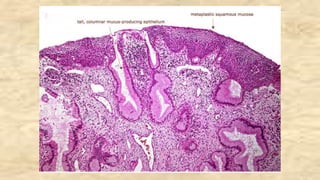
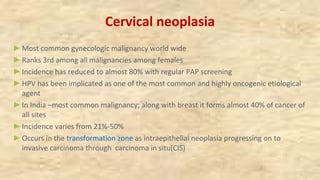
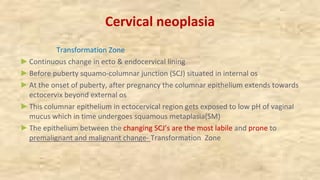
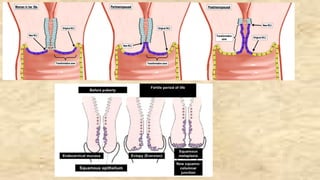
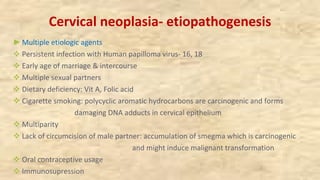
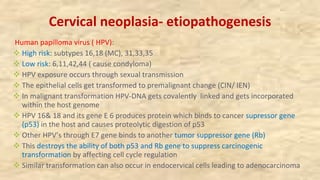
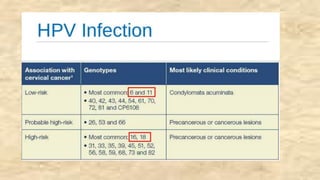
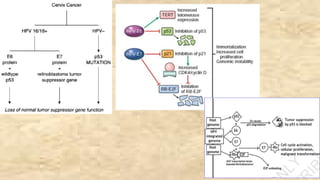
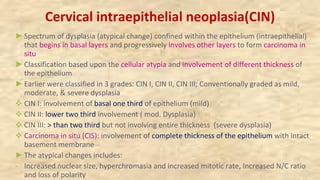
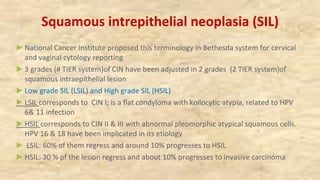
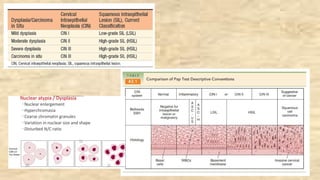
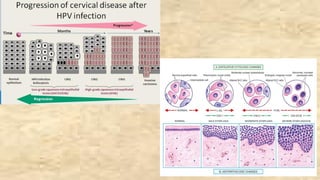
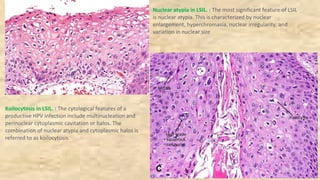
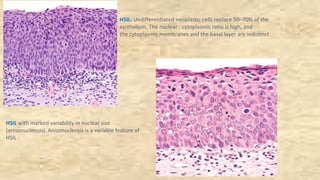
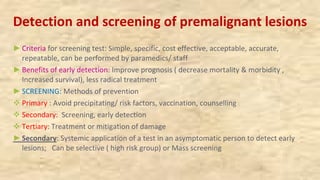
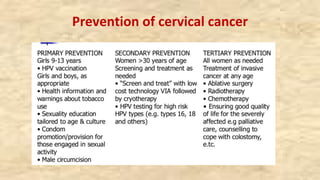
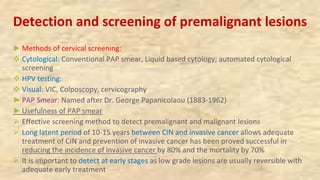
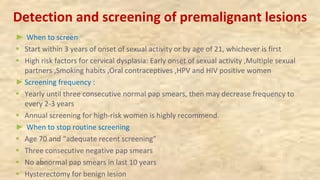
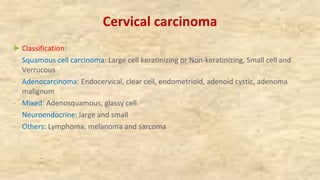
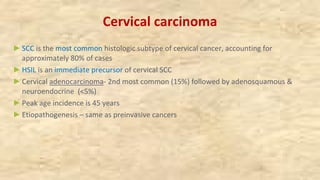
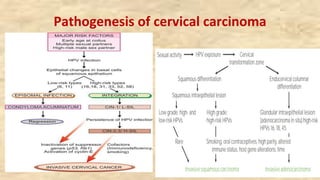
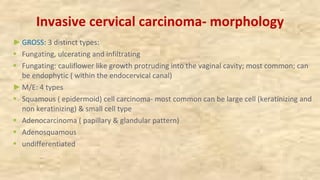
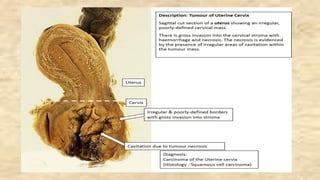
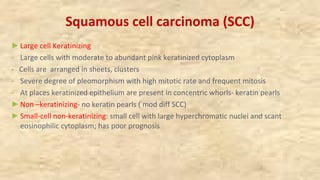
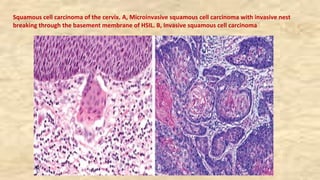
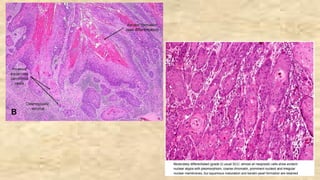
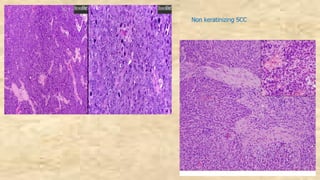
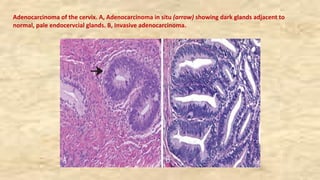
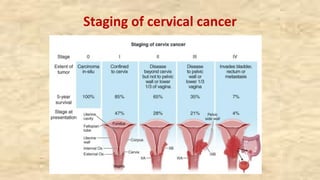
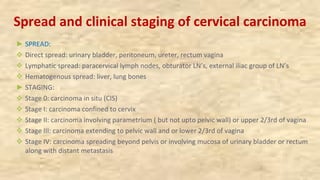
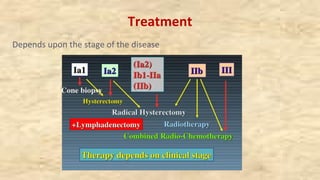
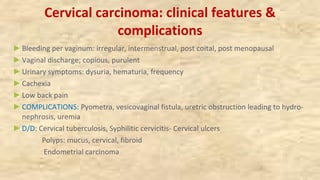
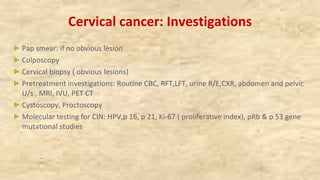
This document discusses pathology of the female genital tract, focusing on cervicitis and carcinoma of the cervix. It describes the etiology, pathogenesis and progression of cervical carcinoma. Cervicitis is usually caused by bacterial or viral infections and presents with inflammation of the cervix. Cervical carcinoma is often associated with HPV infection and develops through premalignant stages of cervical intraepithelial neoplasia. Regular Pap smear screening can detect cervical lesions early and reduce mortality from cervical cancer. The document outlines screening guidelines and pathological features of various cervical lesions, cancers and their staging.