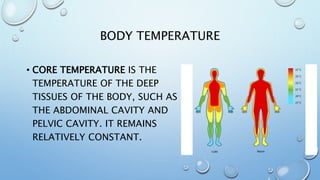
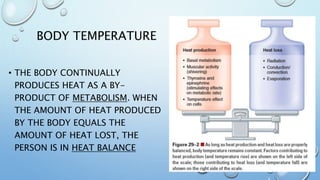
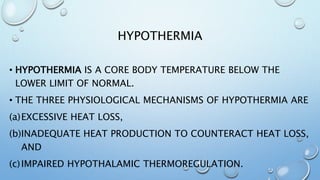
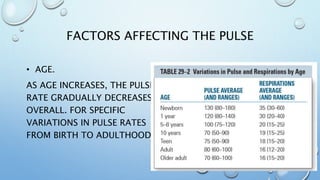
The document provides an overview of health assessments, focusing on vital signs such as body temperature, pulse, respiration, and blood pressure. It explains the importance of these measurements in monitoring health, discusses factors affecting body temperature and pulse, outlines types of fevers, and offers nursing interventions for managing abnormal temperature conditions like hypothermia and fever. Additionally, it details methods and sites for measuring body temperature and pulse, as well as factors influencing these vital signs.





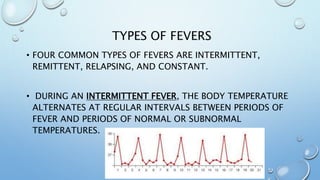
![TYPES OF FEVERS
• DURING A REMITTENT FEVER SUCH AS WITH A COLD OR
INFLUENZA, A WIDE RANGE OF TEMPERATURE
FLUCTUATIONS (MORE THAN 2°C [3.6°F]) OCCURS OVER A
24-HOUR PERIOD, ALL OF WHICH ARE ABOVE NORMAL.](https://image.slidesharecdn.com/04vitalsignstemppulse-190318152313/85/04-vital-signs-temp-pulse-34-320.jpg)

![ALTERATIONS IN BODY TEMPERATURE
• HEAT EXHAUSTION IS A RESULT OF EXCESSIVE HEAT AND
DEHYDRATION. SIGNS OF HEAT EXHAUSTION INCLUDE
PALENESS, DIZZINESS, NAUSEA, VOMITING, FAINTING,
AND A MODERATELY INCREASED TEMPERATURE (38.3°C
TO 38.9°C [101°F TO 102°F]).](https://image.slidesharecdn.com/04vitalsignstemppulse-190318152313/85/04-vital-signs-temp-pulse-40-320.jpg)







![REFERENCES
• AUDREY BERMAN . . . [ET AL.]. – 9TH ED. (2012)
KOZIER & ERB’S FUNDAMENTALS OF NURSING
CONCEPTS, PROCESS, AND PRACTICE.
• BICKLEY, LYNN S. -11TH ED. (2013) BATES’ GUIDE
TO PHYSICAL EXAMINATION AND HISTORY-
TAKING.](https://image.slidesharecdn.com/04vitalsignstemppulse-190318152313/85/04-vital-signs-temp-pulse-104-320.jpg)