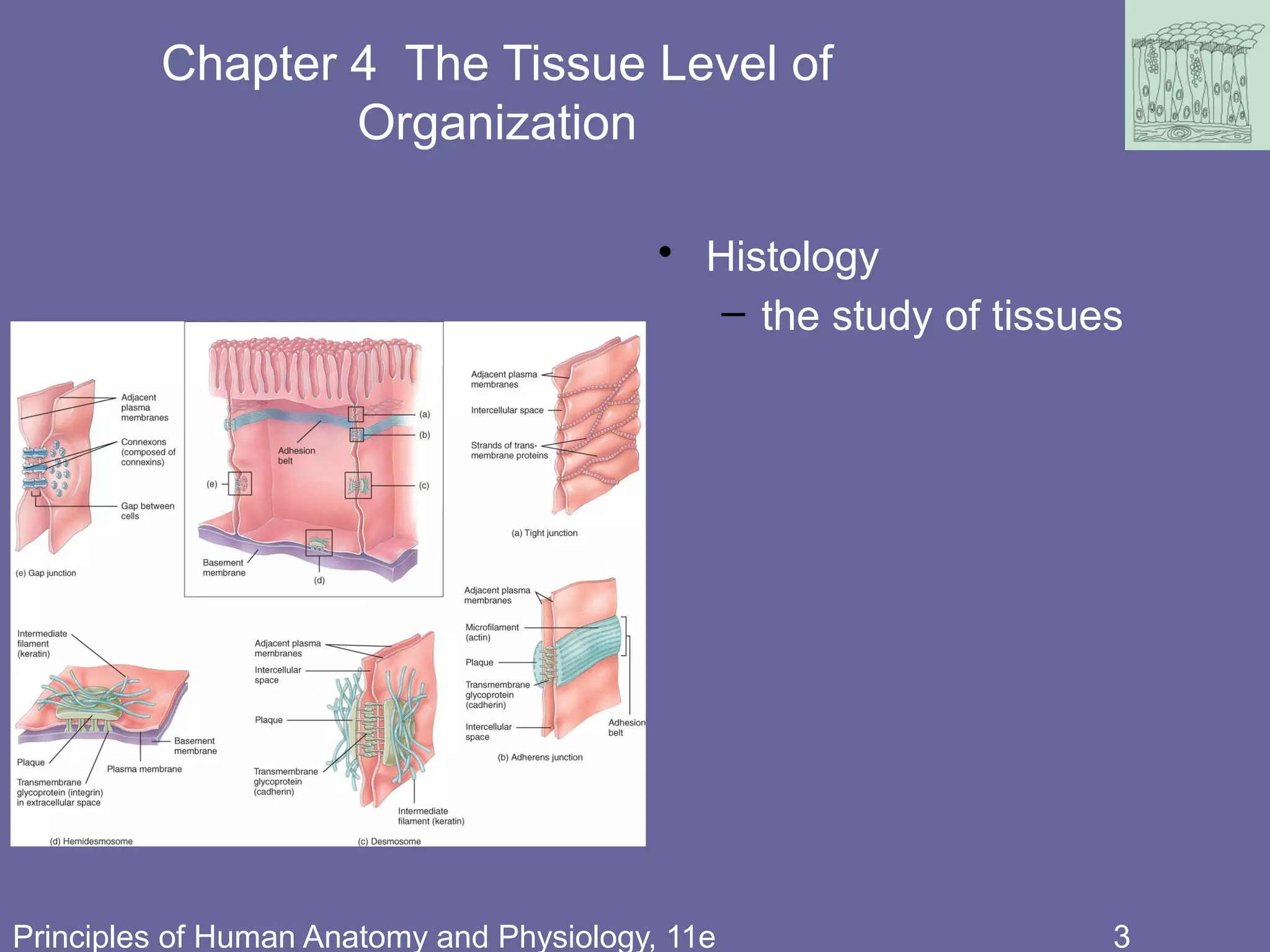
This document discusses the different types of tissues in the human body. It begins by defining what a tissue is and describing the four main types: epithelial, connective, muscle and nervous tissue. It then focuses on epithelial tissues, describing the different classifications of epithelium based on cell shape and layering. Simple epithelia are one cell layer thick, while stratified epithelia have two or more layers. Specific examples of each epithelial type are provided, along with diagrams to illustrate their structure.