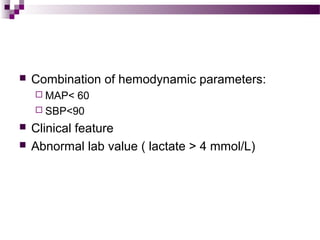
1) Shock is defined as inadequate tissue perfusion resulting from low blood pressure and abnormal cellular metabolism. The main types of shock are hypovolemic, distributive, and cardiogenic.
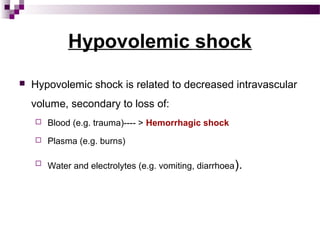
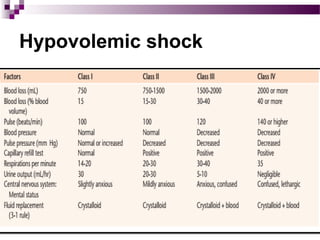
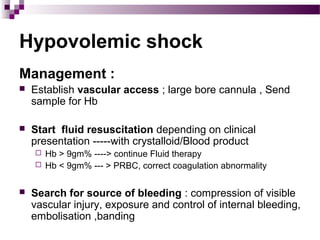
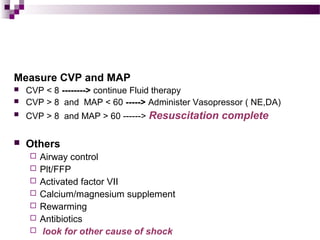
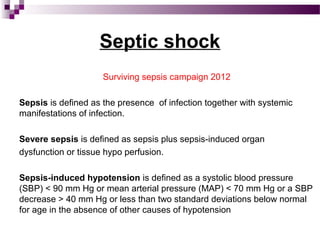
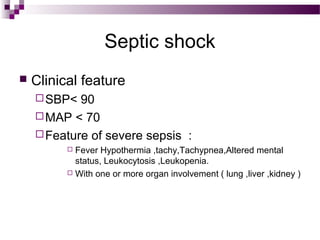
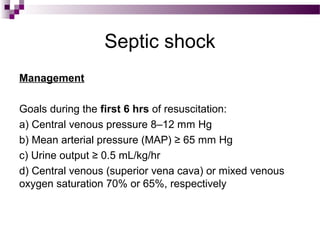
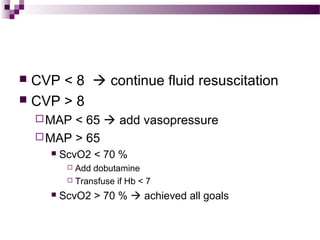
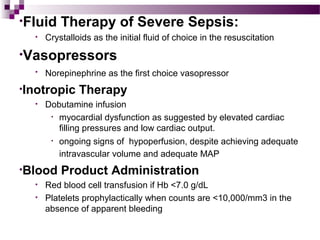
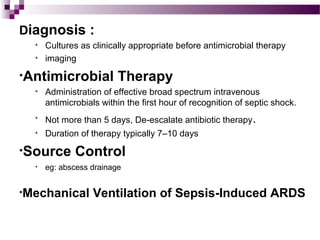
2) Hypovolemic shock occurs when intravascular volume is decreased, such as from blood loss, and requires fluid resuscitation. Septic shock, a form of distributive shock, involves infection and organ dysfunction and responds to antibiotics, fluids, and vasopressors.
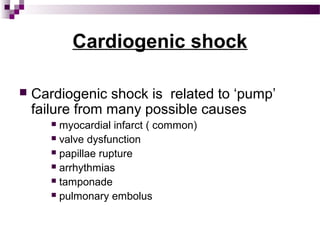
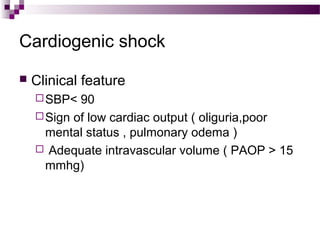
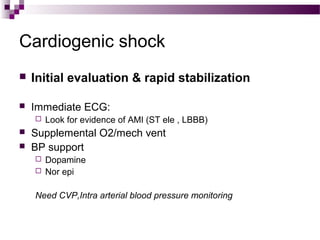
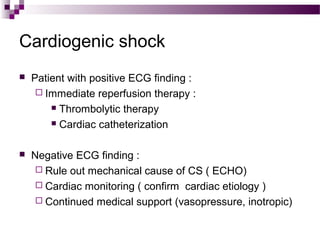
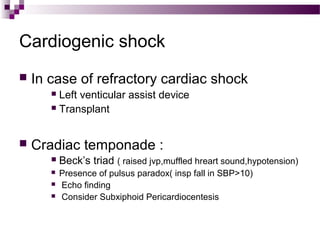
3) Cardiogenic shock results from heart failure or damage and may be caused by myocardial infarction. It requires hemodynamic support through medications like dopamine or norepinephrine while the underlying cardiac issue is addressed.