Embed presentation
Downloaded 25 times

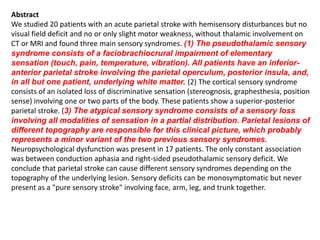
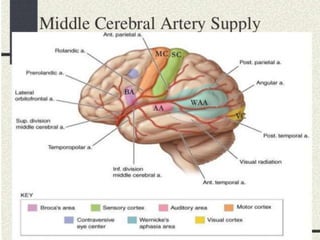
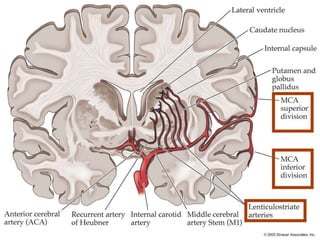

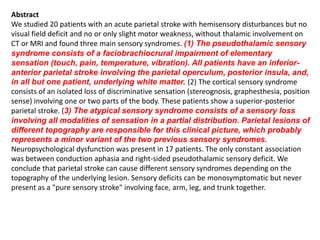
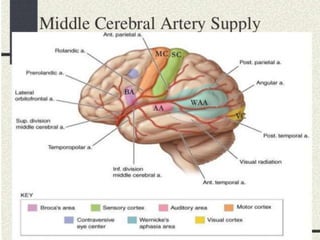
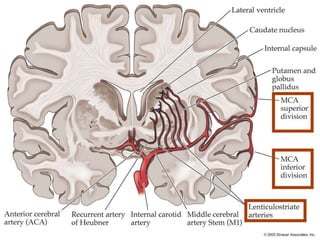
Three main sensory syndromes can result from parietal stroke: 1) Pseudothalamic sensory syndrome involving elementary sensation loss in the face, arm, and leg, caused by anterior-inferior parietal lesions including the parietal operculum and posterior insula. 2) Cortical sensory syndrome of isolated discriminative sensation loss in one or two body parts, from superior-posterior parietal lesions. 3) Atypical sensory syndrome with sensory loss across all modalities in a partial body distribution, from variably located parietal lesions, representing a minor variant of the first two syndromes. Neuropsychological dysfunction was present in most patients.