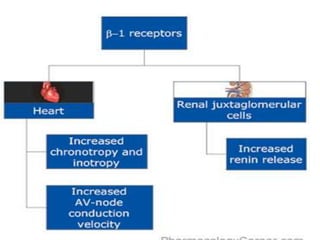
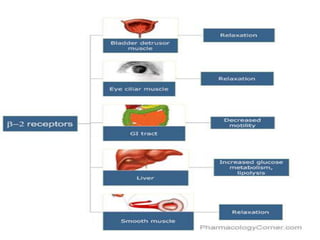
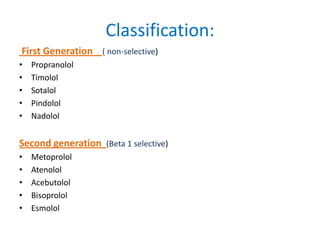
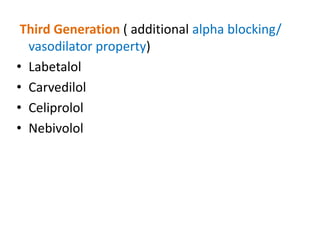
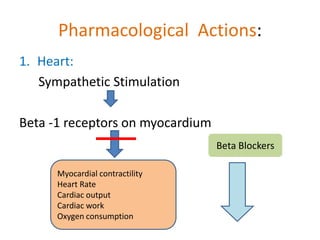
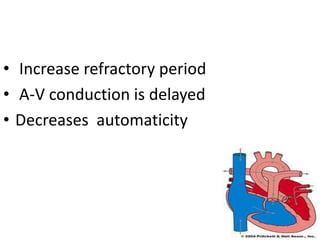
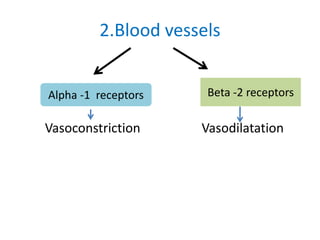
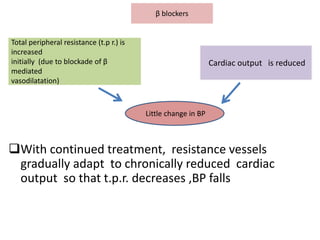
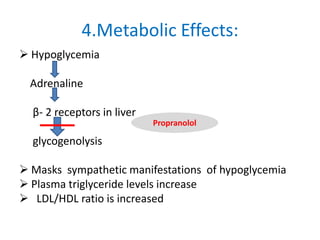
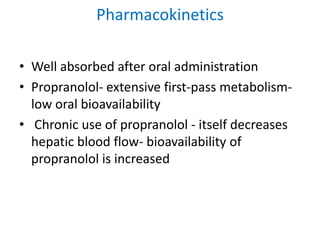
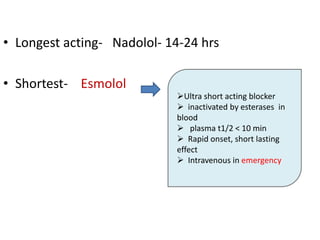
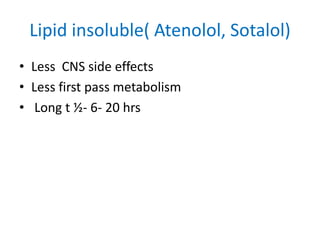
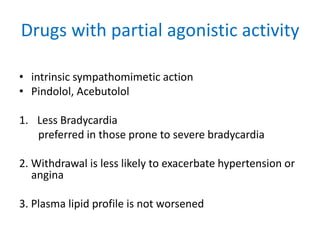
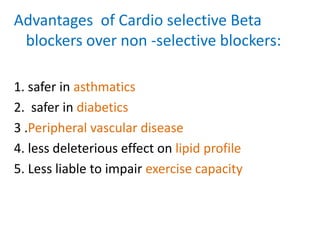
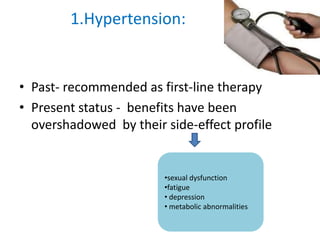
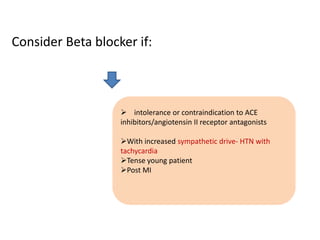
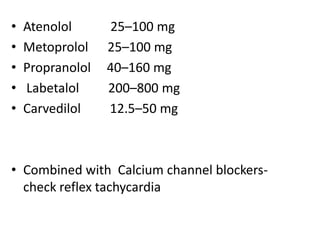
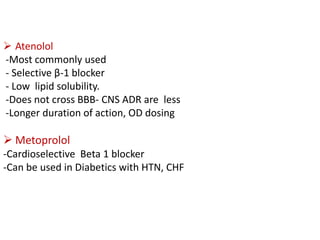
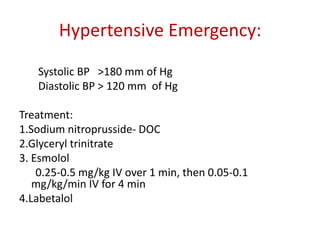
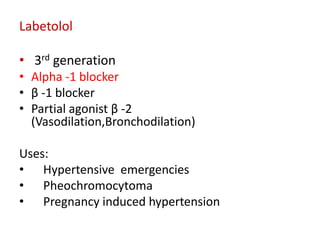
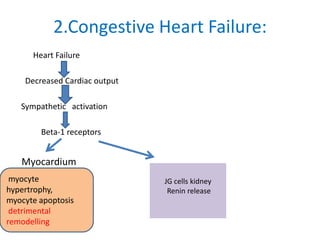
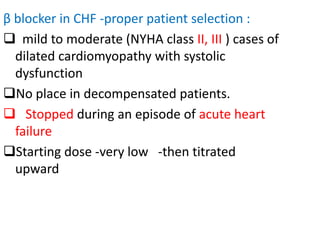
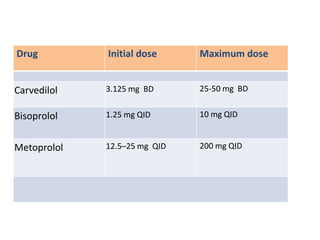
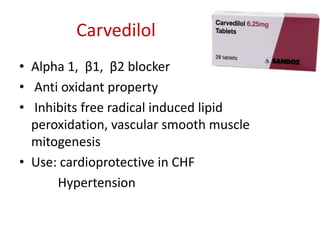
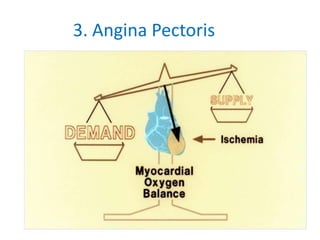
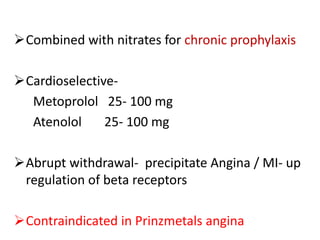
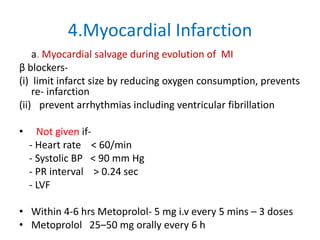
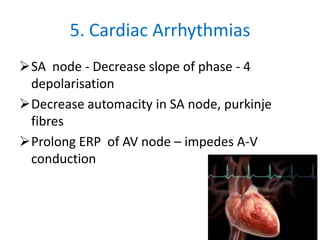
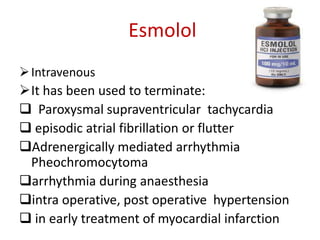
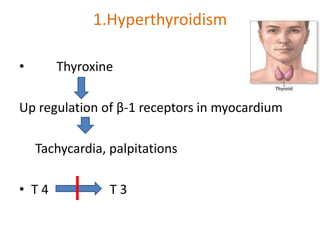
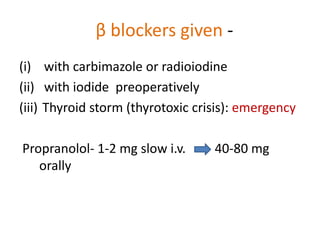
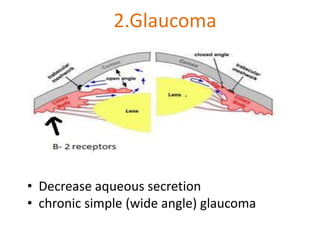
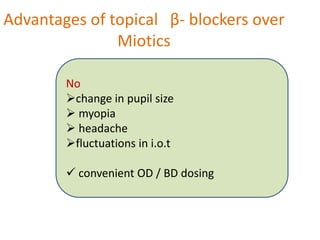
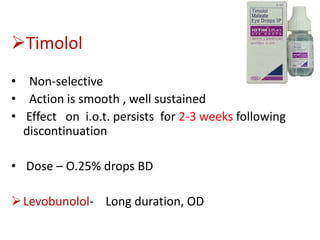
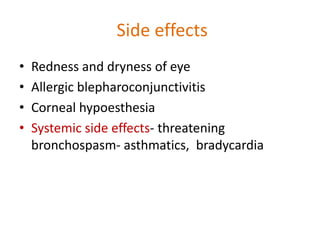
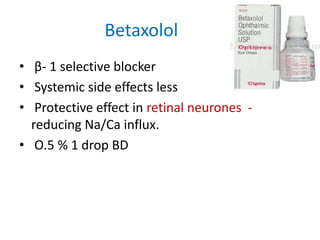
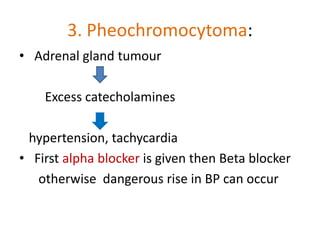
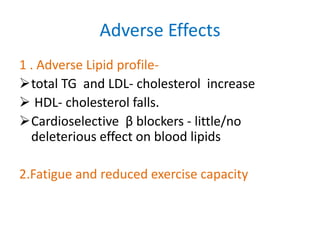
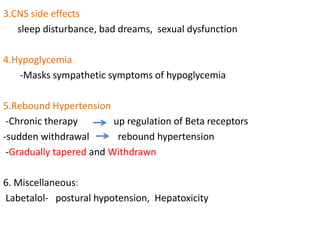
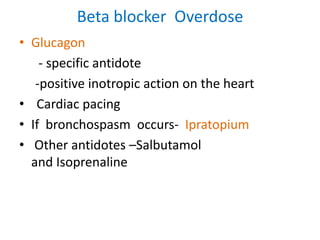
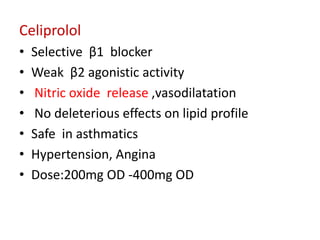
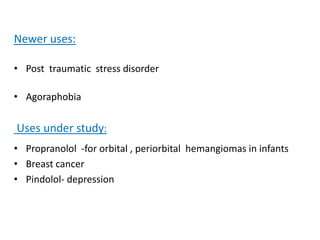
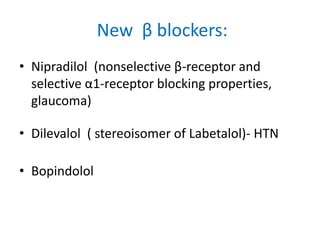
Beta receptor blockers are a class of drugs that are commonly used to treat cardiovascular conditions by blocking beta-1 and beta-2 receptors. They have several therapeutic uses including hypertension, congestive heart failure, angina, myocardial infarction, and cardiac arrhythmias. They work by decreasing heart rate, contractility, and blood pressure. Common side effects include fatigue, bronchospasm, and metabolic abnormalities. First generation blockers are non-selective while later generations are more cardioselective. Carvedilol is used for heart failure, atenolol for hypertension, and esmolol for emergencies. Propranolol is effective for migraine prevention. Timolol eye drops are used for glaucoma treatment by decreasing