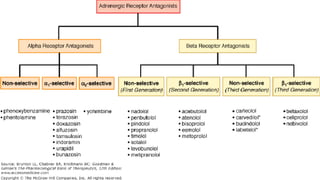
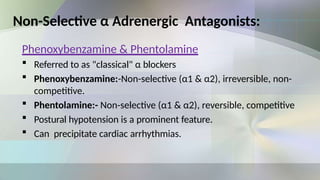
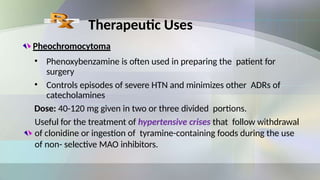
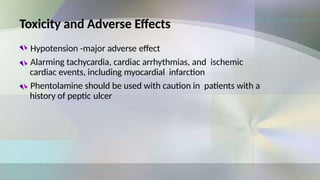
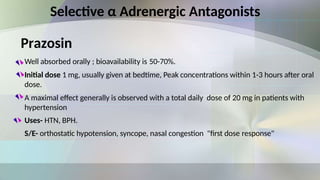
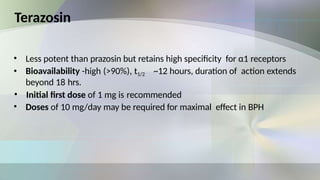
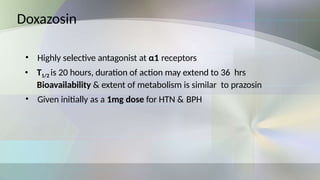
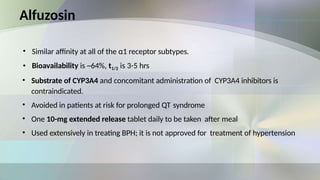
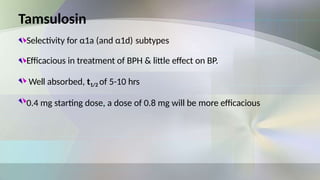
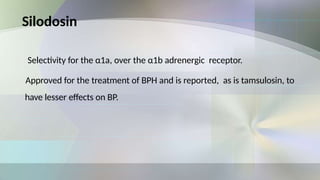
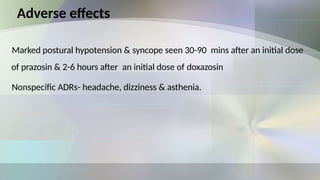
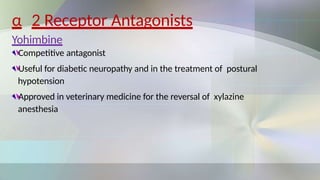
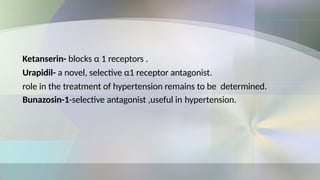
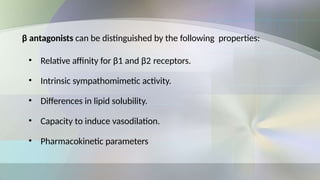
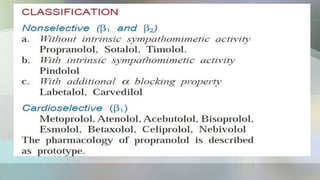
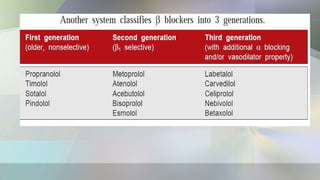
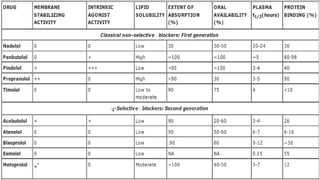
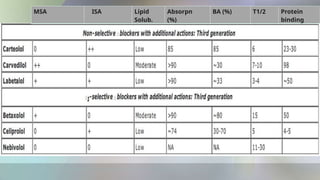
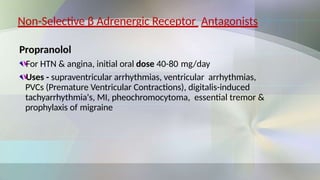
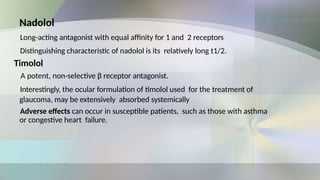
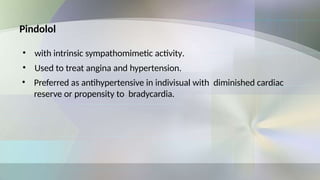
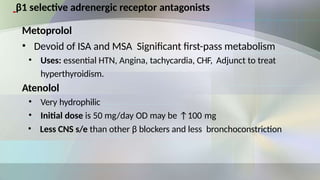
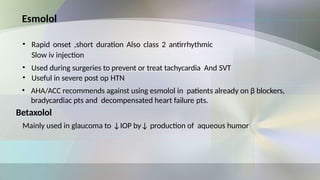
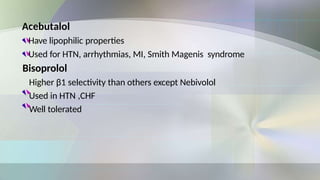
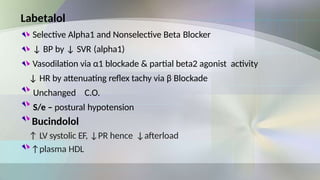
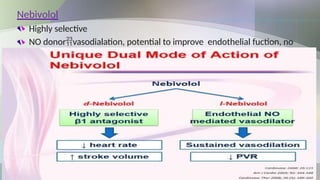
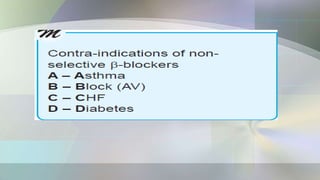
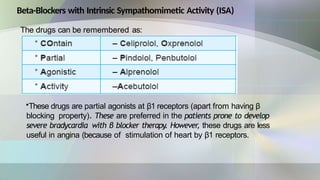
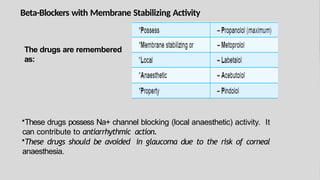
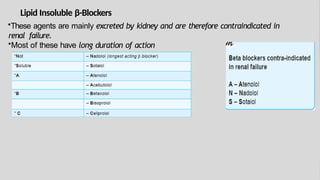
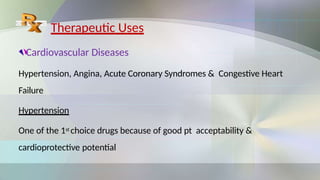
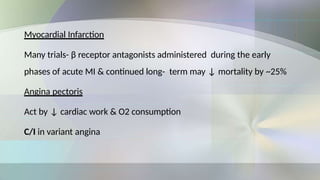
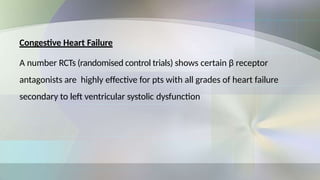
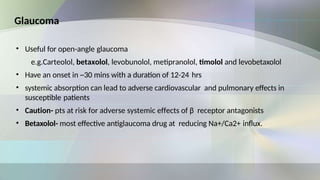
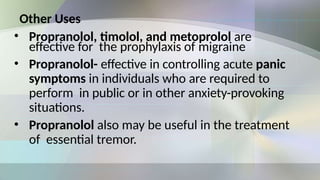
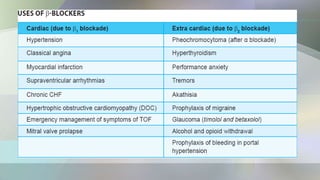
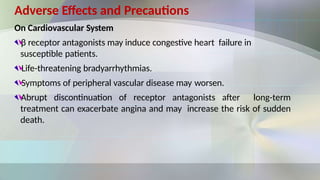
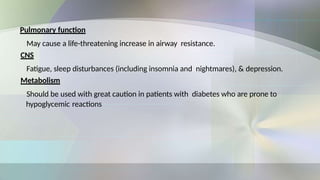
The document provides an overview of autonomic nervous system drugs focusing on sympathetic nervous system sympatholytics, specifically adrenergic antagonists. It details the classifications, therapeutic uses, adverse effects, and dosing guidelines for various α and β adrenergic blocking agents, such as phenoxybenzamine, propranolol, and their selective variants. Additionally, it discusses the implications of these medications in treating conditions like hypertension, angina, and heart failure, along with potential adverse effects and precautions.