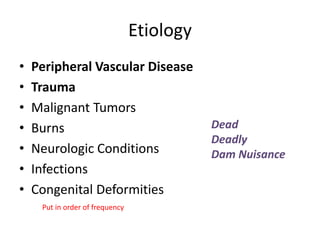
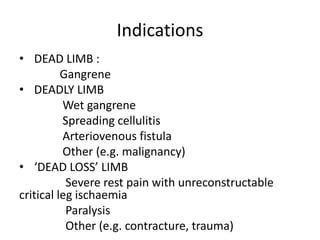
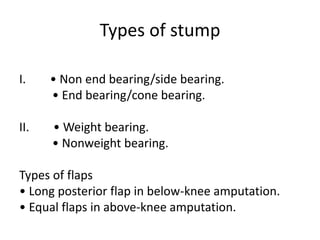
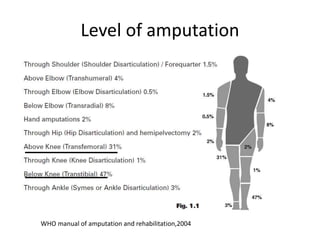
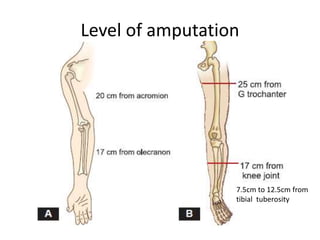
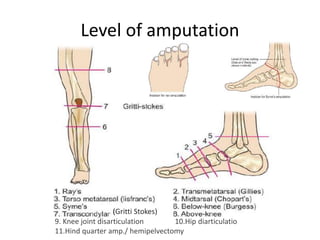
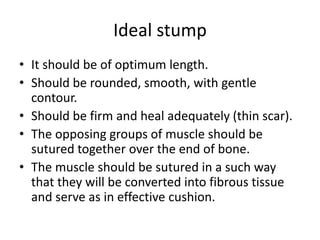
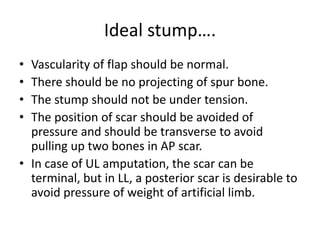
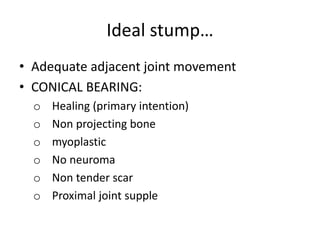
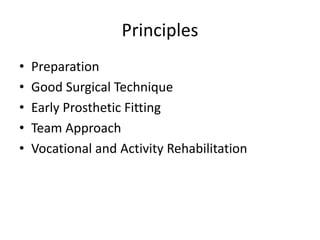
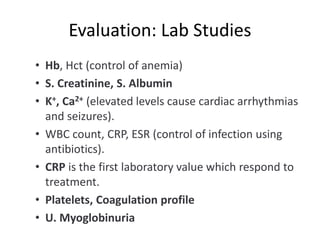
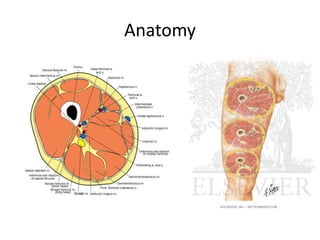
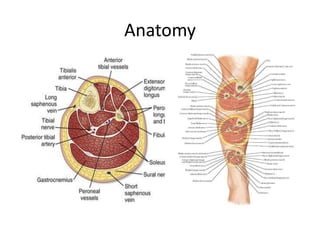
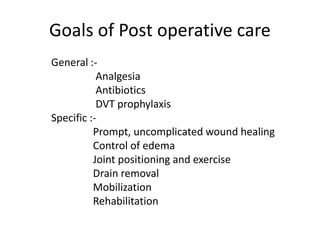
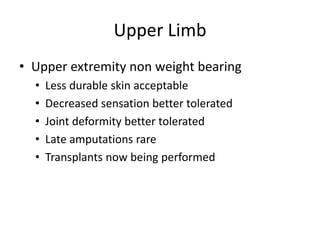
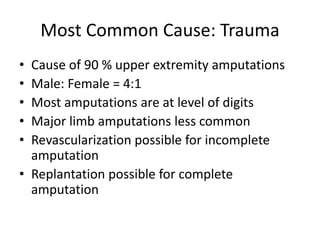
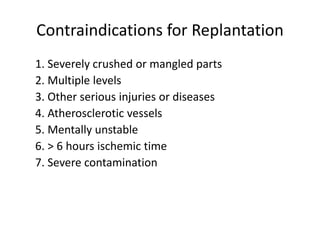
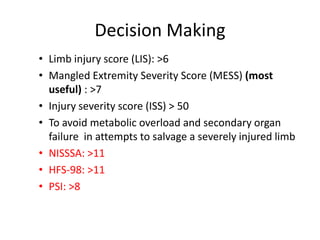
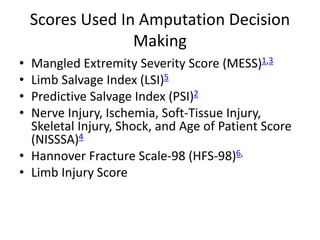
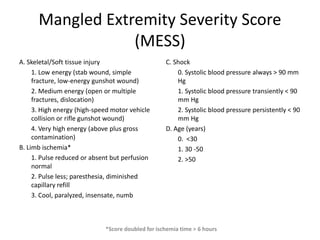
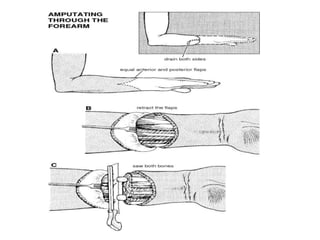
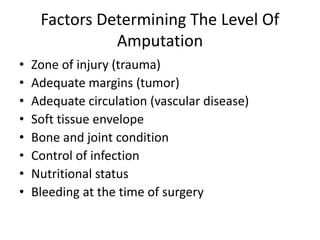
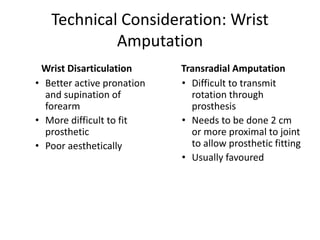
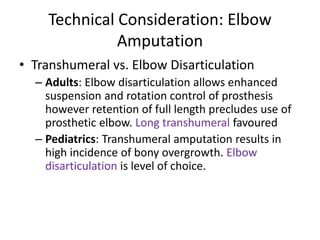
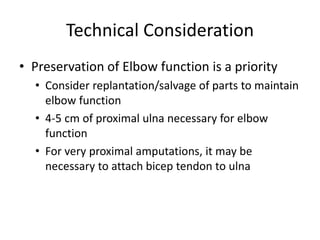
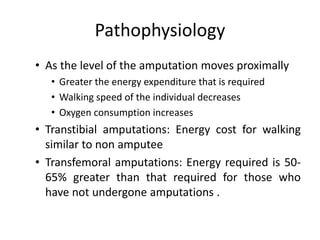
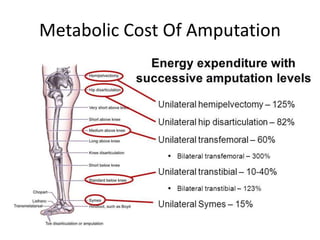
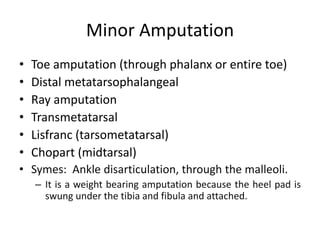
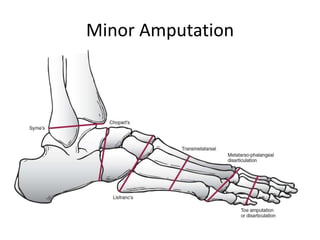
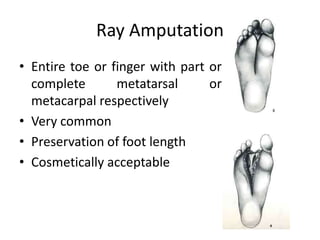
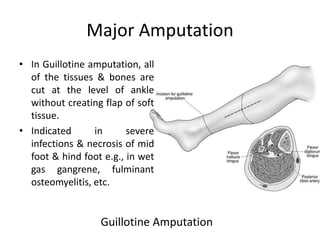
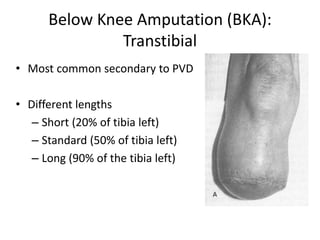
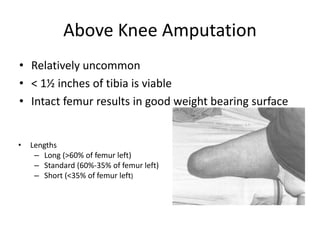
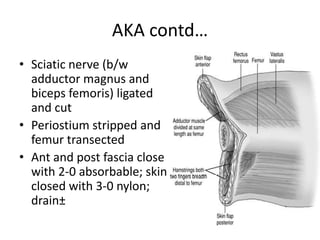
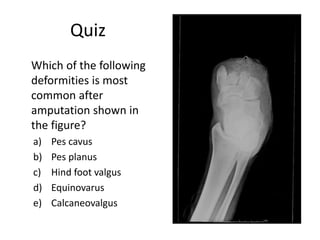
This document provides an overview of amputation and rehabilitation. It discusses the history and definitions of amputation, as well as pre-operative preparations and evaluations. The document outlines different types and levels of amputations for both upper and lower limbs. Key principles of amputation surgery are described, including goals for post-operative care and rehabilitation. Specific considerations for upper limb amputations are also covered.