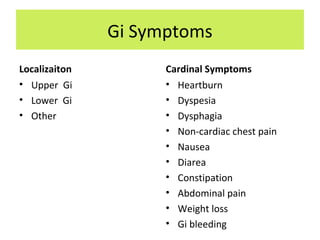
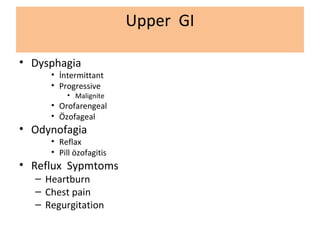
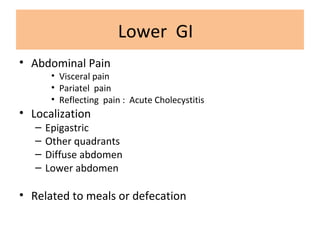
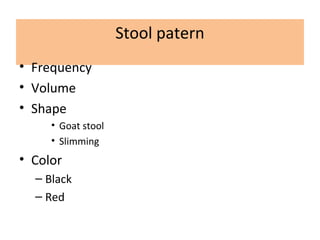
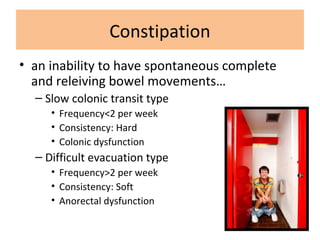
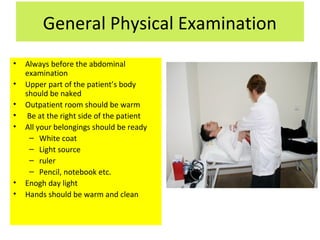
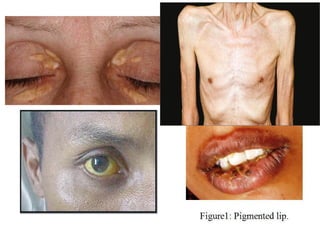
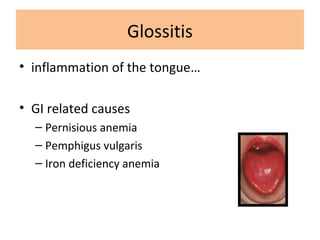
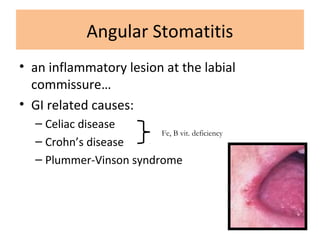
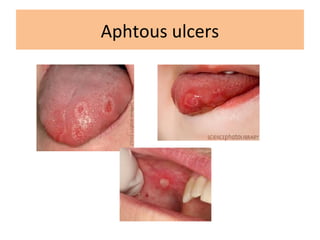
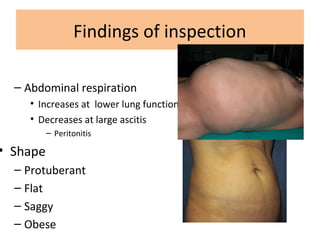
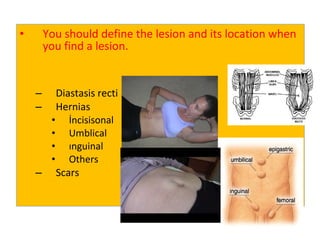
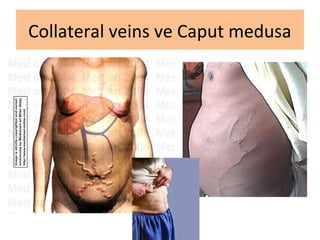
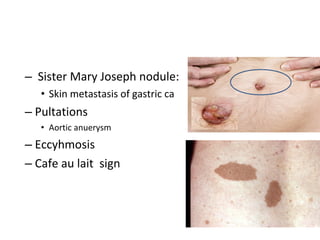
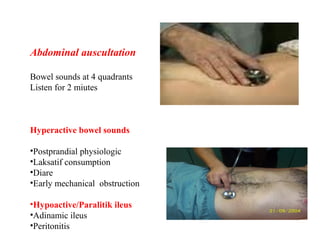
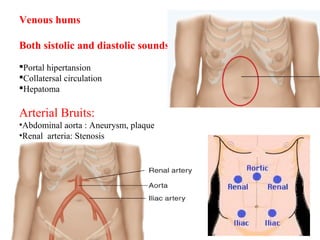
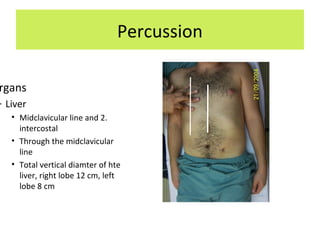
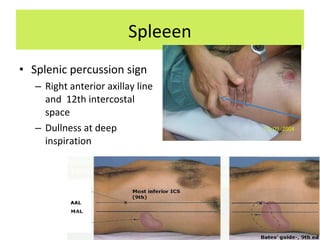
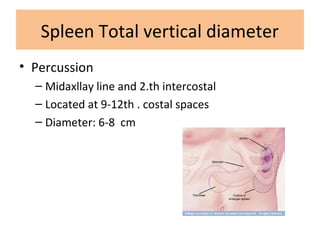
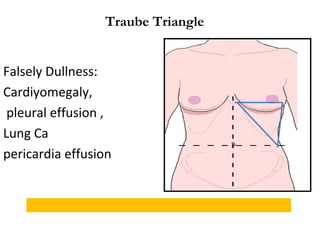
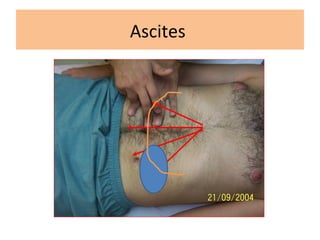
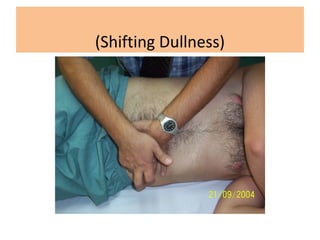
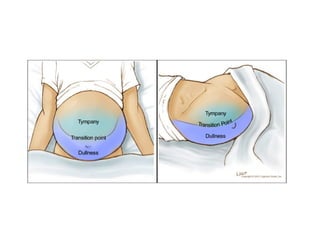
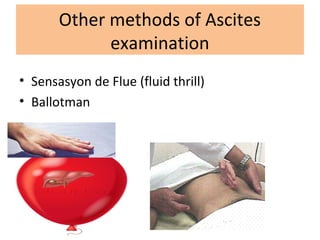
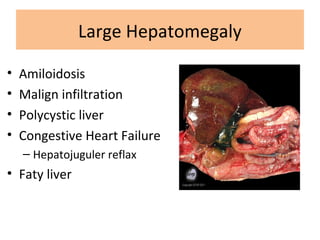
This document provides an overview of abdominal examination techniques and findings. It discusses approaching gastrointestinal symptoms, performing a general physical exam, and specifically examining the abdomen through inspection, auscultation, percussion, and palpation. Key areas of the abdomen that can be examined include the liver, spleen, kidneys, gallbladder, and pancreas. Specific examination findings are outlined that may indicate various gastrointestinal conditions. The importance of thorough abdominal exams to evaluate symptoms and guide diagnosis is emphasized.