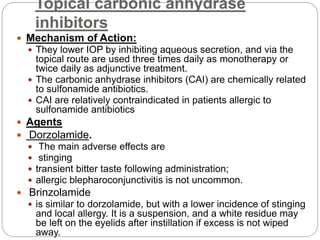
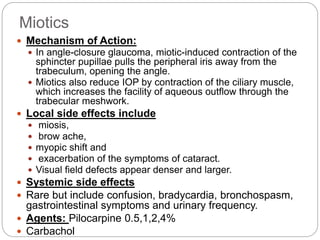
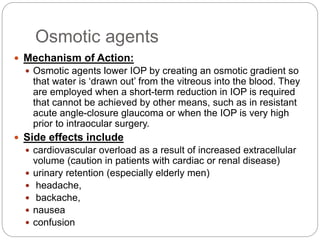
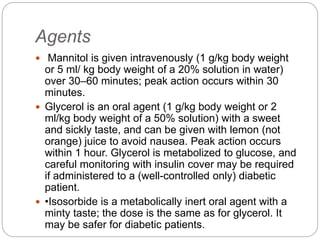
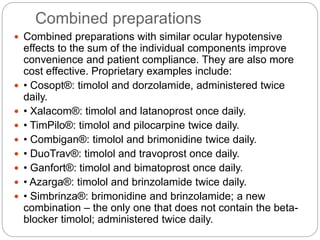
This document discusses various medical treatments for glaucoma, including topical eye drop medications from different drug classes. It describes the mechanisms of action, administration, efficacy and side effects of prostaglandin analogues, beta blockers, carbonic anhydrase inhibitors, alpha-2 agonists, miotics, osmotic agents, and some combination drug preparations. The document provides detailed information on commonly used glaucoma drugs to help clinicians select appropriate treatment options based on a patient's needs and risk factors.