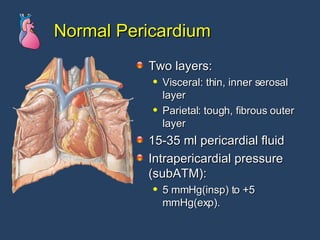
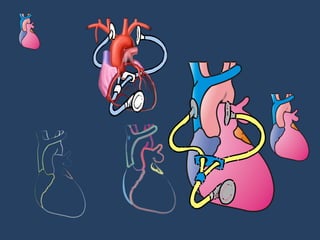
The document discusses various pericardial diseases including normal anatomy, pericarditis, pericardial effusions, cardiac tamponade, and constrictive pericarditis. Key points include:
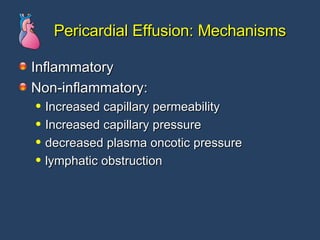
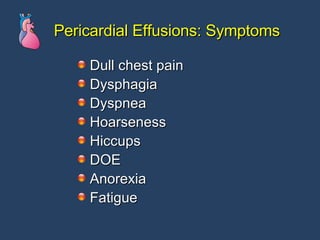
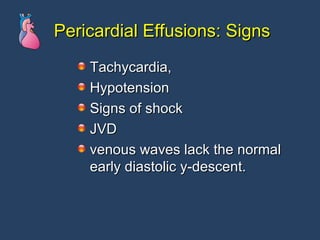
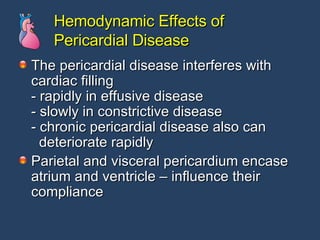
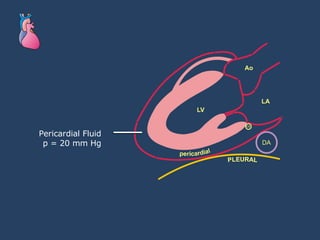
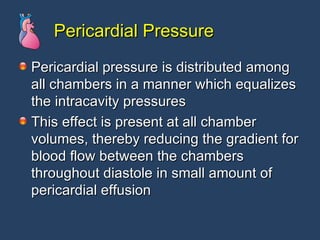
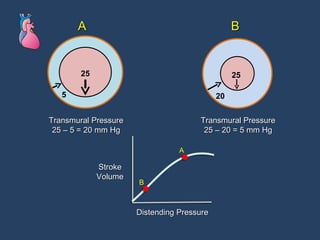
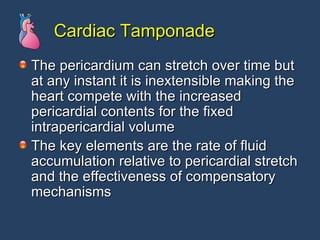
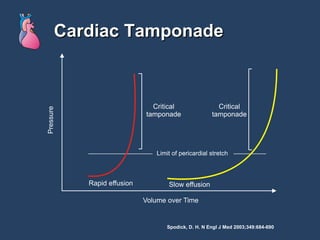
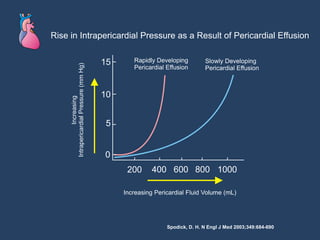
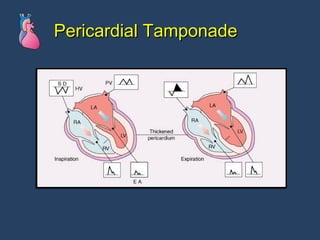
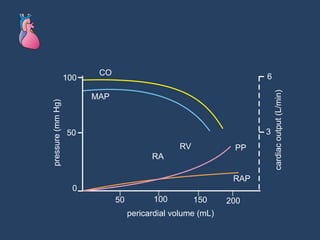
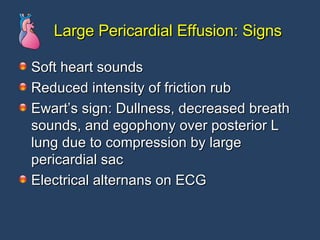
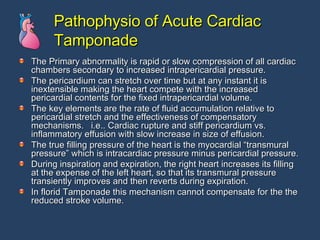
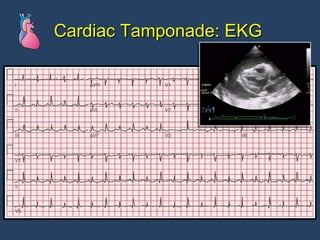
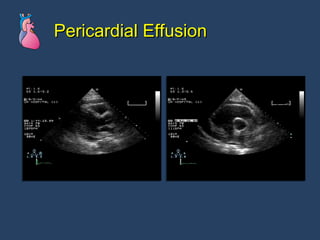
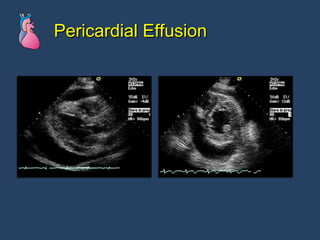
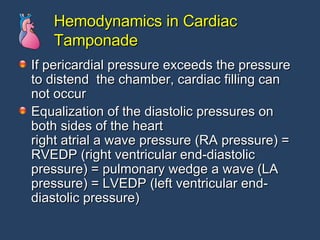
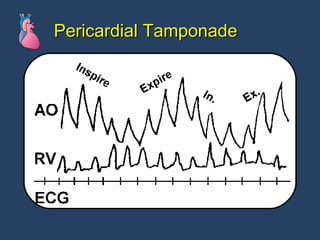
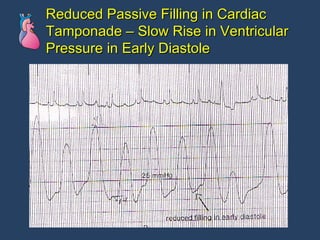
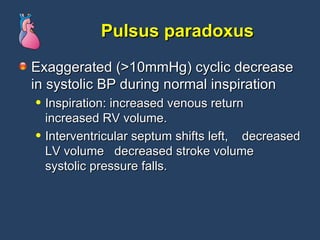
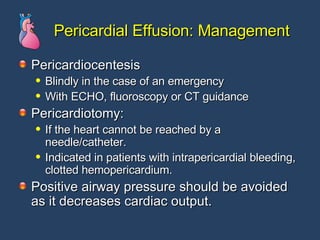
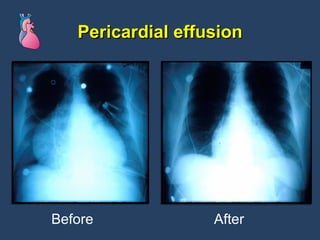
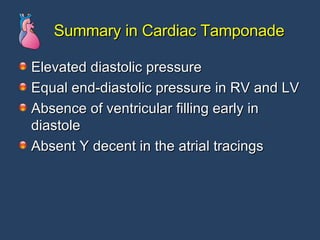
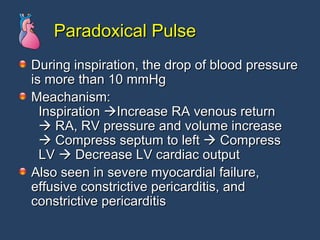
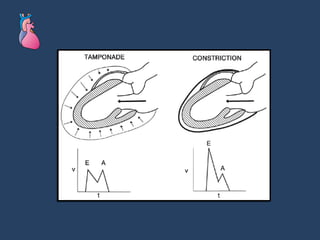
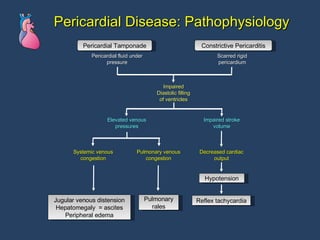
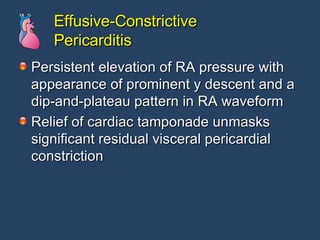
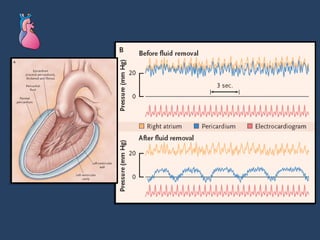
- Pericardial effusions can lead to cardiac tamponade by exerting pressure on the heart and restricting filling.
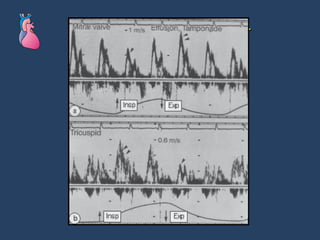
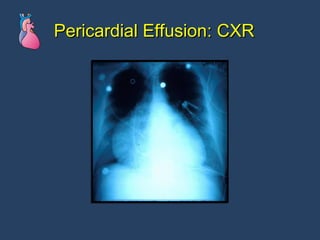
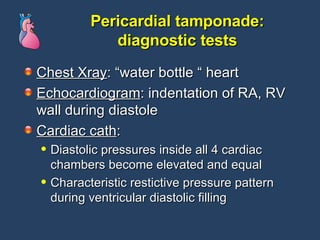
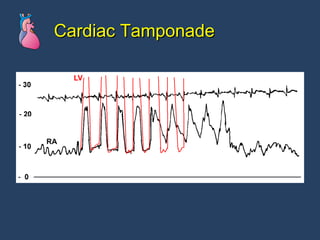
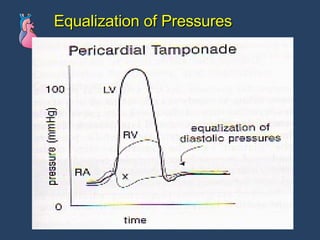
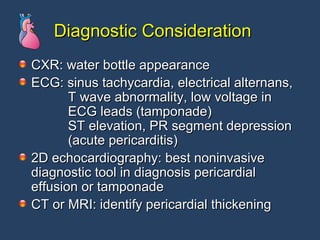
- Cardiac tamponade is diagnosed using echocardiogram, chest x-ray and equalized diastolic pressures on catheterization.
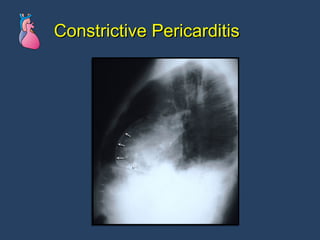
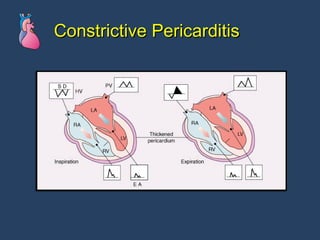
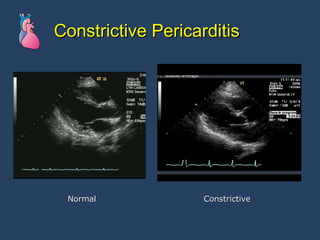
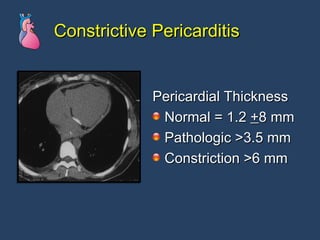
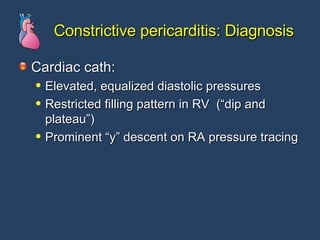
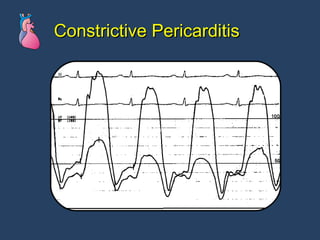
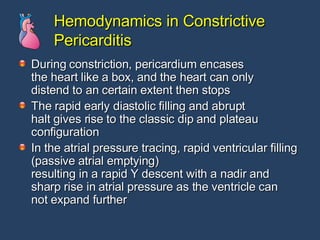
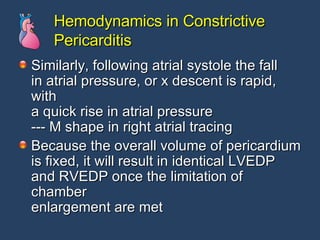
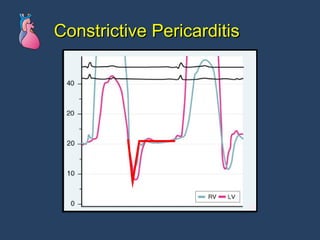
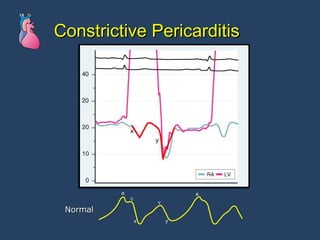
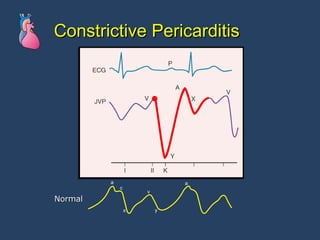
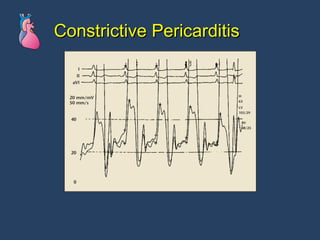
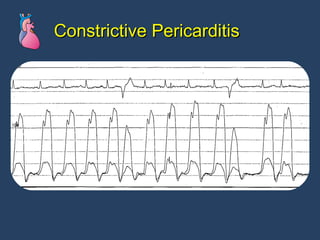
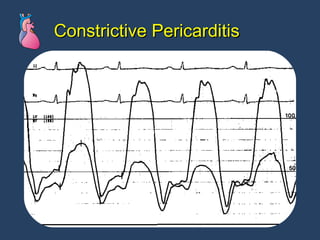
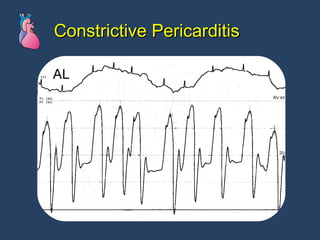
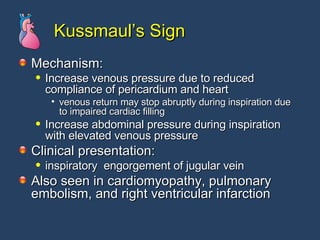
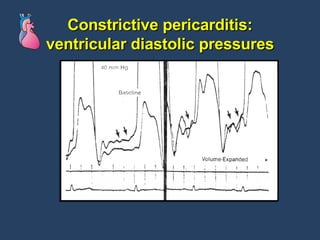
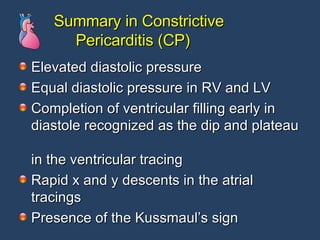
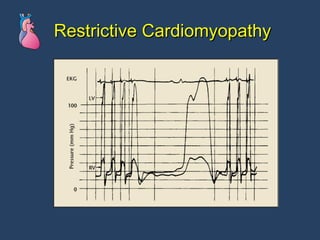
- Constrictive pericarditis involves thickened pericardium constraining all chambers and is diagnosed using characteristic hemodynamic tracings on catheterization.