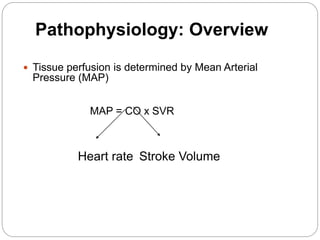
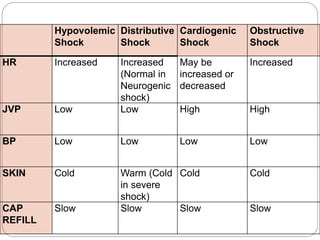
This document provides an overview of shock, including its history, definitions, types, pathophysiology, signs and symptoms, and management. It discusses the four main types of shock - cardiogenic, obstructive, hypovolemic, and distributive - describing the insult, physiologic effects, and compensatory mechanisms for each. Treatment of shock focuses on the ABCDE approach - airway, breathing, circulation, disability, and exposure. Restoring adequate circulation through fluid resuscitation is key. The goals of treatment are to optimize oxygen delivery and achieve endpoints of resuscitation like urine output and hemodynamic parameters.




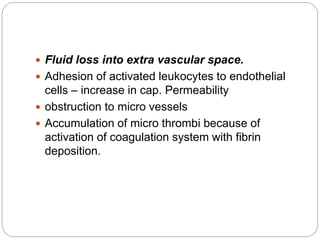
![IRREVERSIBLE
IF HYPOPERFUSION CONTINUES
HYPOXIA – ANAEROBIC METABOLISM
INCREASE IN LACTIC ACID + INCREASE [H+]
DECREASE IN CAP. HYDR. PRES
INCREASE IN POST CAP. SPHINCTER TONE
WEAKENING OF PRE CAP SPHINCTER TONE
FLUID MOVES INTO EXTRA VASCULAR SPACE](https://image.slidesharecdn.com/shock-150602065701-lva1-app6892/85/shock-6-320.jpg)






















































![Blood Product Administration
PRBC transfusion if Hb <7.0 g/dL ; target 7.0-
9.0 g/dL.
Erythropoietin only accepted reasons for
administration of erythropoietin such as renal
failure induced anemia.
No Routine use of fresh frozen plasma to
correct laboratory clotting abnormal
Platelets administered <5,000/mm3 (5 x
109/L) regardless of apparent bleeding.
Higher platelet counts (>50,000/mm3 [50 x
109/L])for surgery or invasive procedures](https://image.slidesharecdn.com/shock-150602065701-lva1-app6892/85/shock-67-320.jpg)