1. Hemorrhagic shock is the most common cause of shock in surgical or trauma patients and results from blood loss that exceeds 15% of circulating volume.
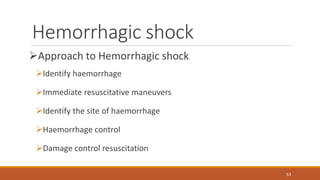
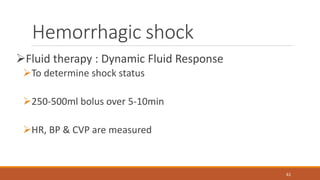
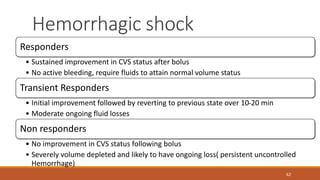
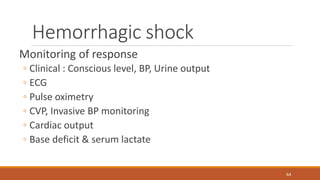
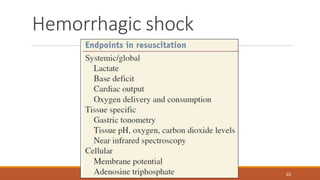
2. Initial management of hemorrhagic shock involves identifying the source of bleeding, providing immediate resuscitation with fluids and blood products, and controlling hemorrhage.
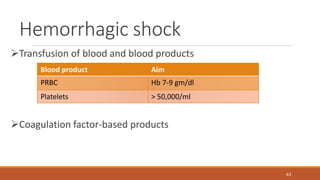
3. Damage control resuscitation principles are followed, including permissive hypotension to limit blood loss and balanced use of crystalloids, colloids, platelets, and plasma to prevent coagulopathy.


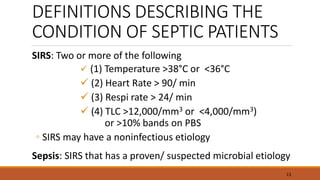
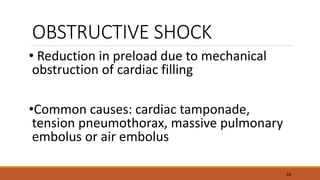







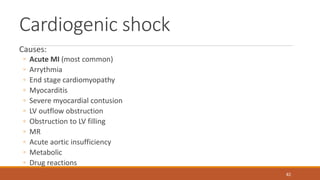

![Obstructive shock
Causes:
◦ Tension Pneumothorax
◦ Pericardial Tamponade
◦ Pulmonary embolus
◦ IVC obstruction [Gravid uterus, DVT, Neoplasm]
◦ Increased Intra-thoracic pressure [ Excess end-expiratory pressure, Neoplasm]
87](https://image.slidesharecdn.com/shockpresentation-160119164451/85/Shock-Pathophysiology-Clinical-Features-Management-79-320.jpg)