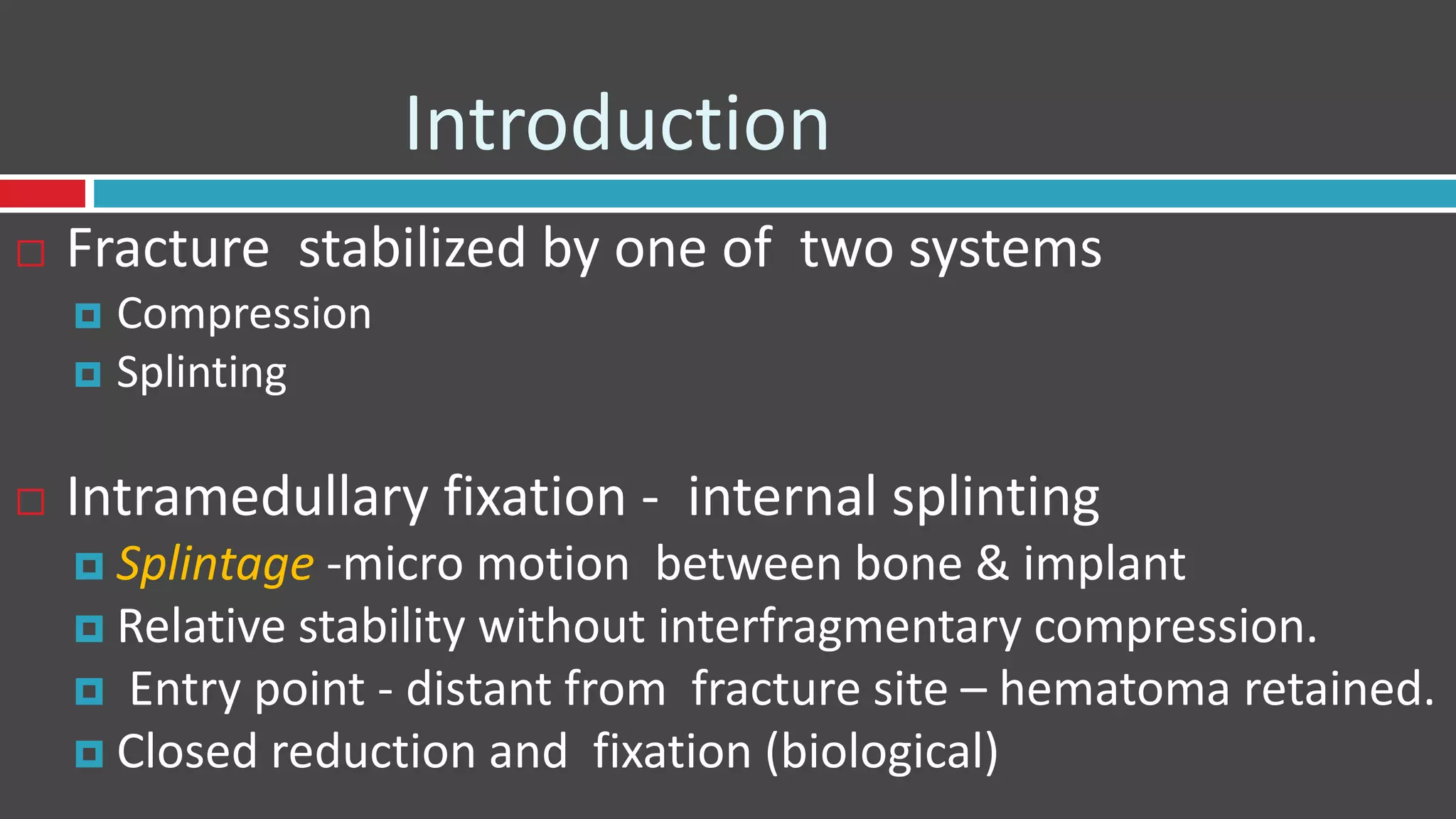
This document provides an overview of intramedullary nailing, including:
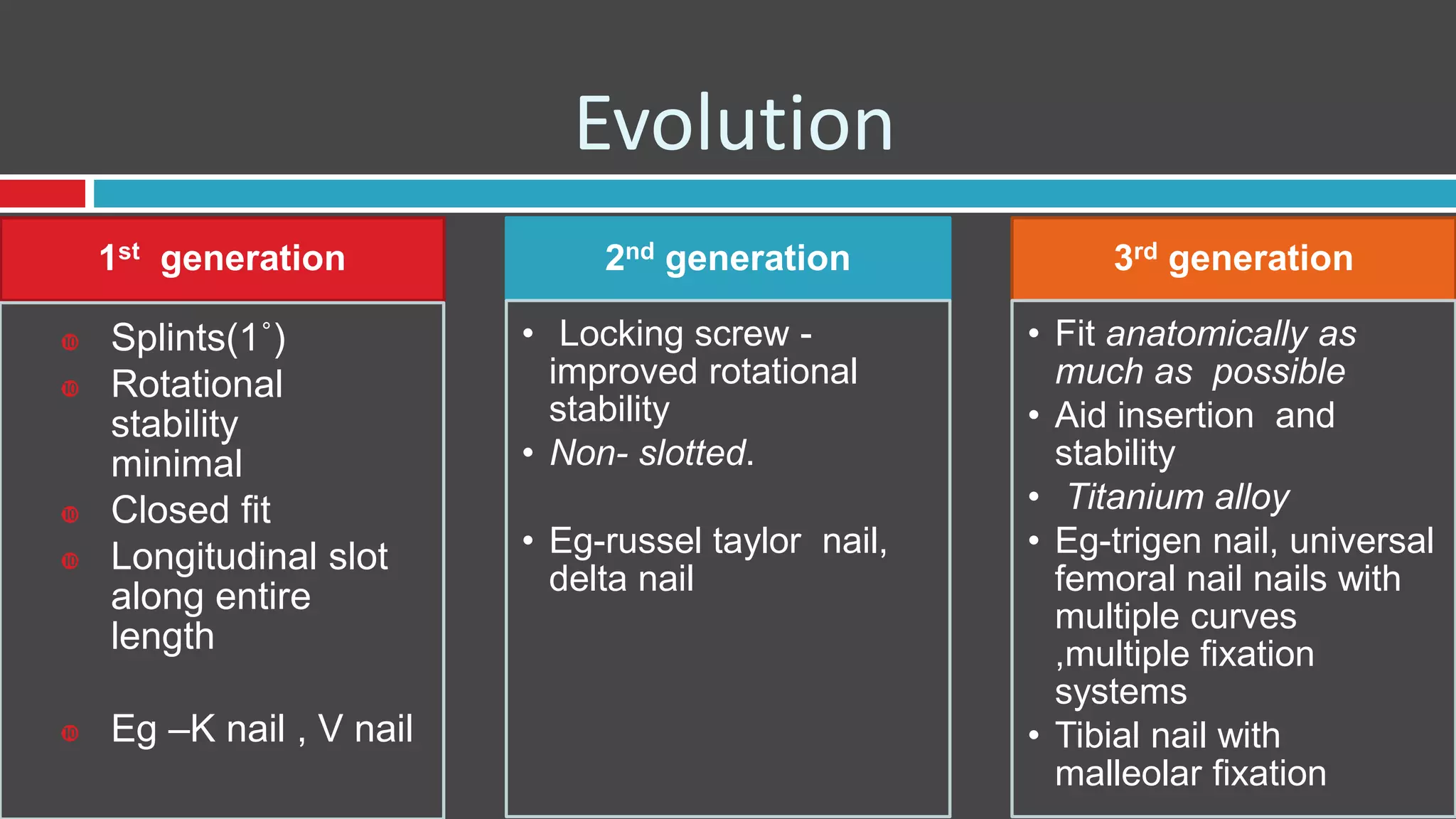
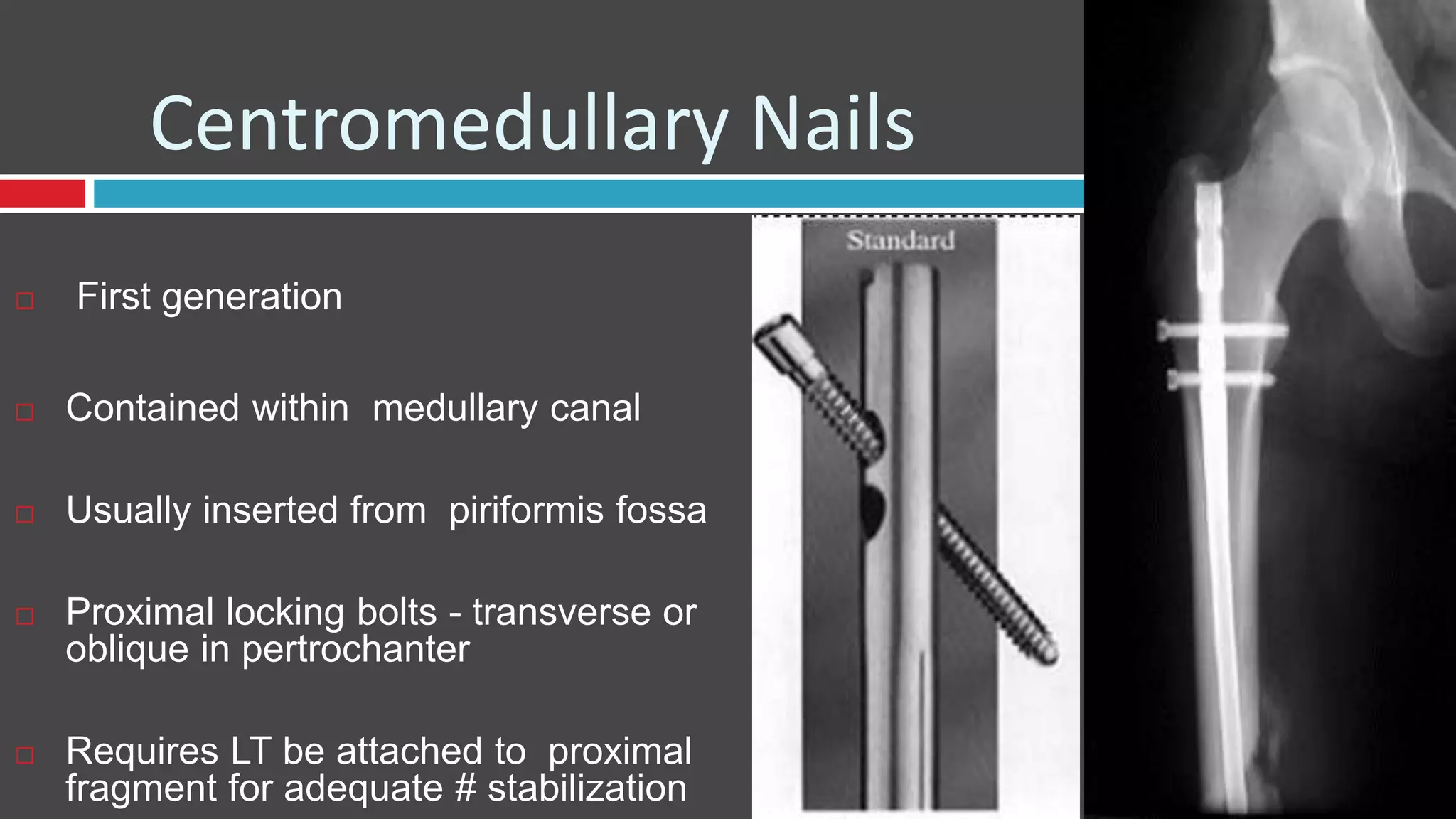
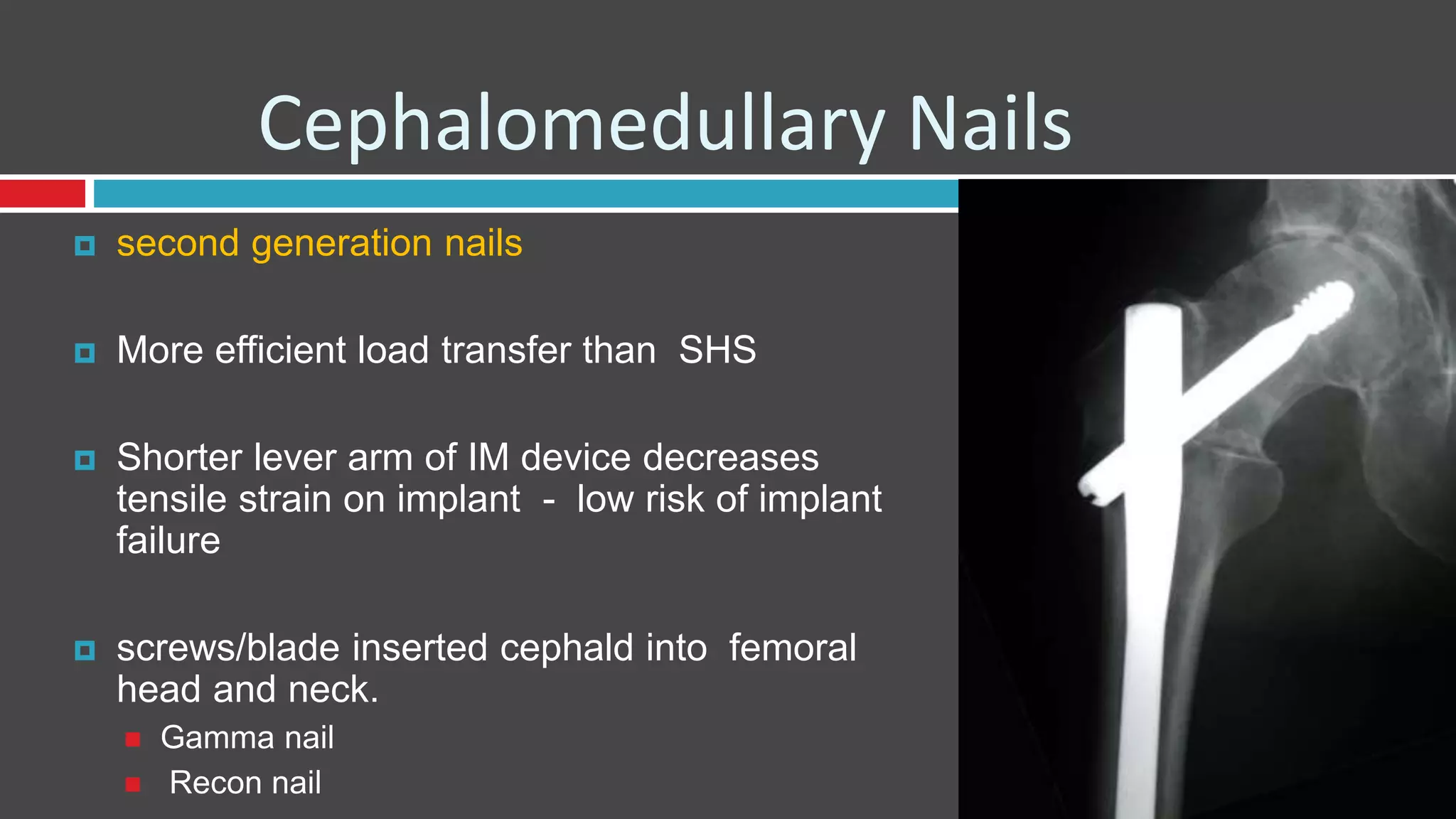
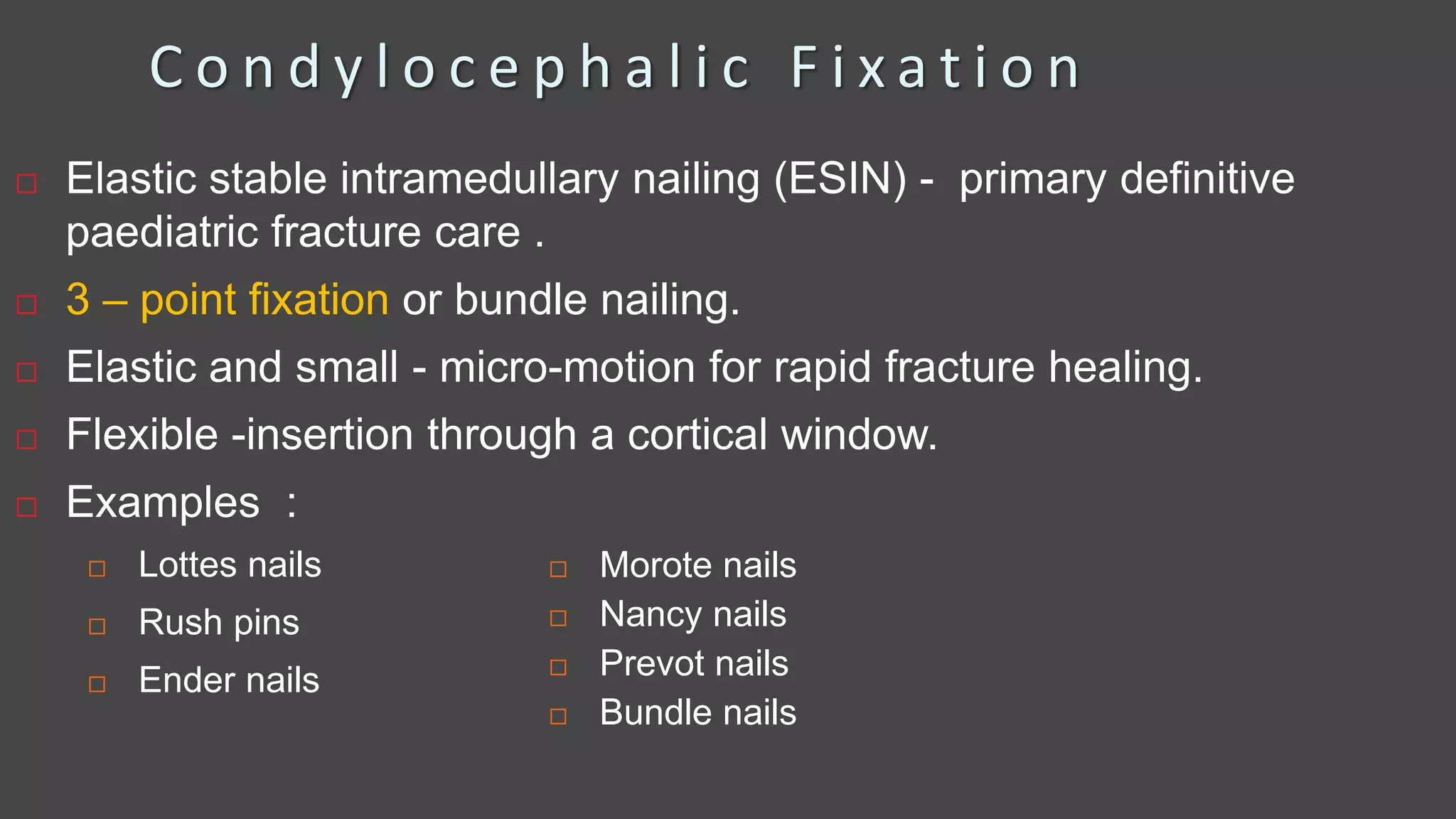
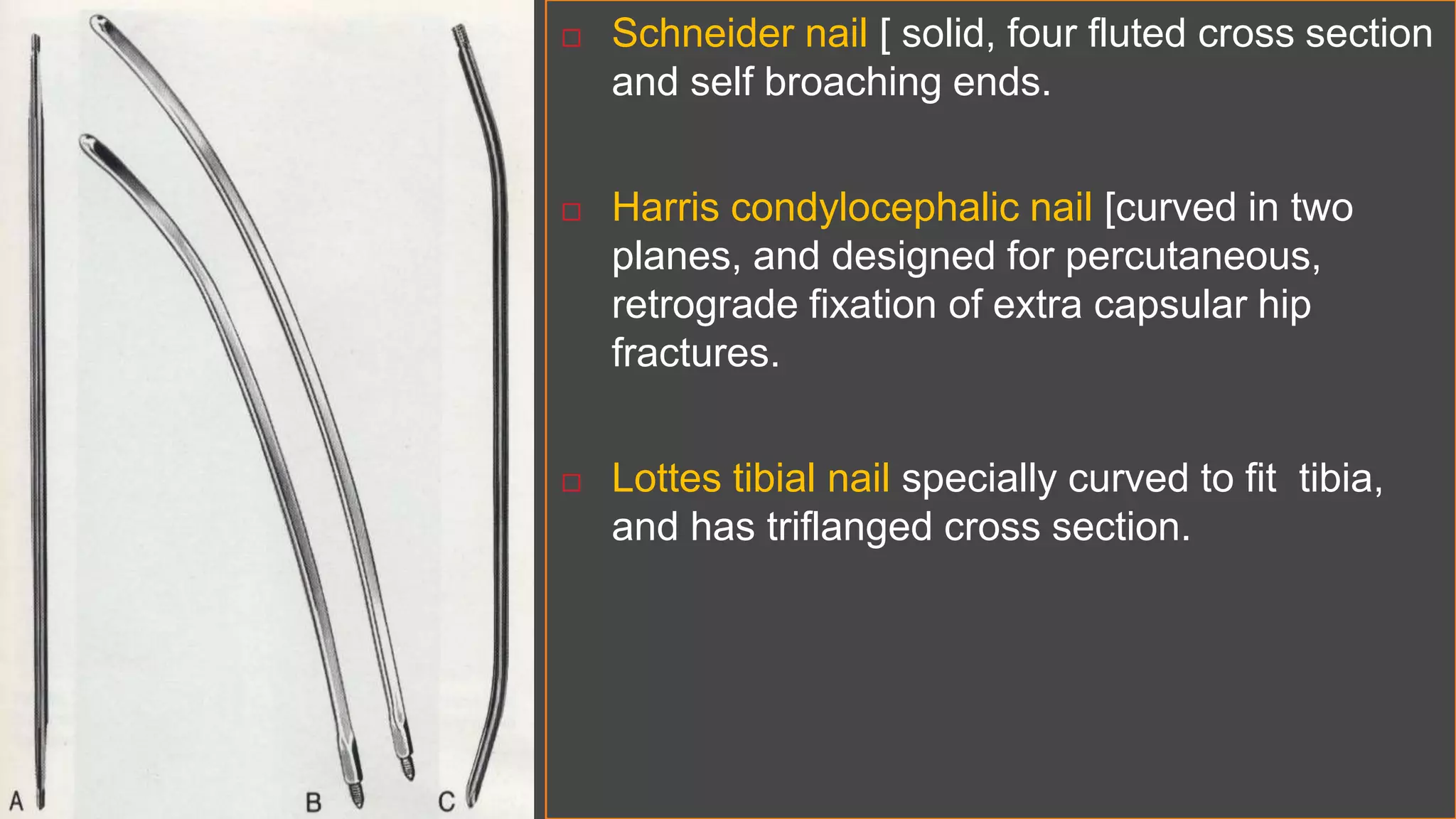
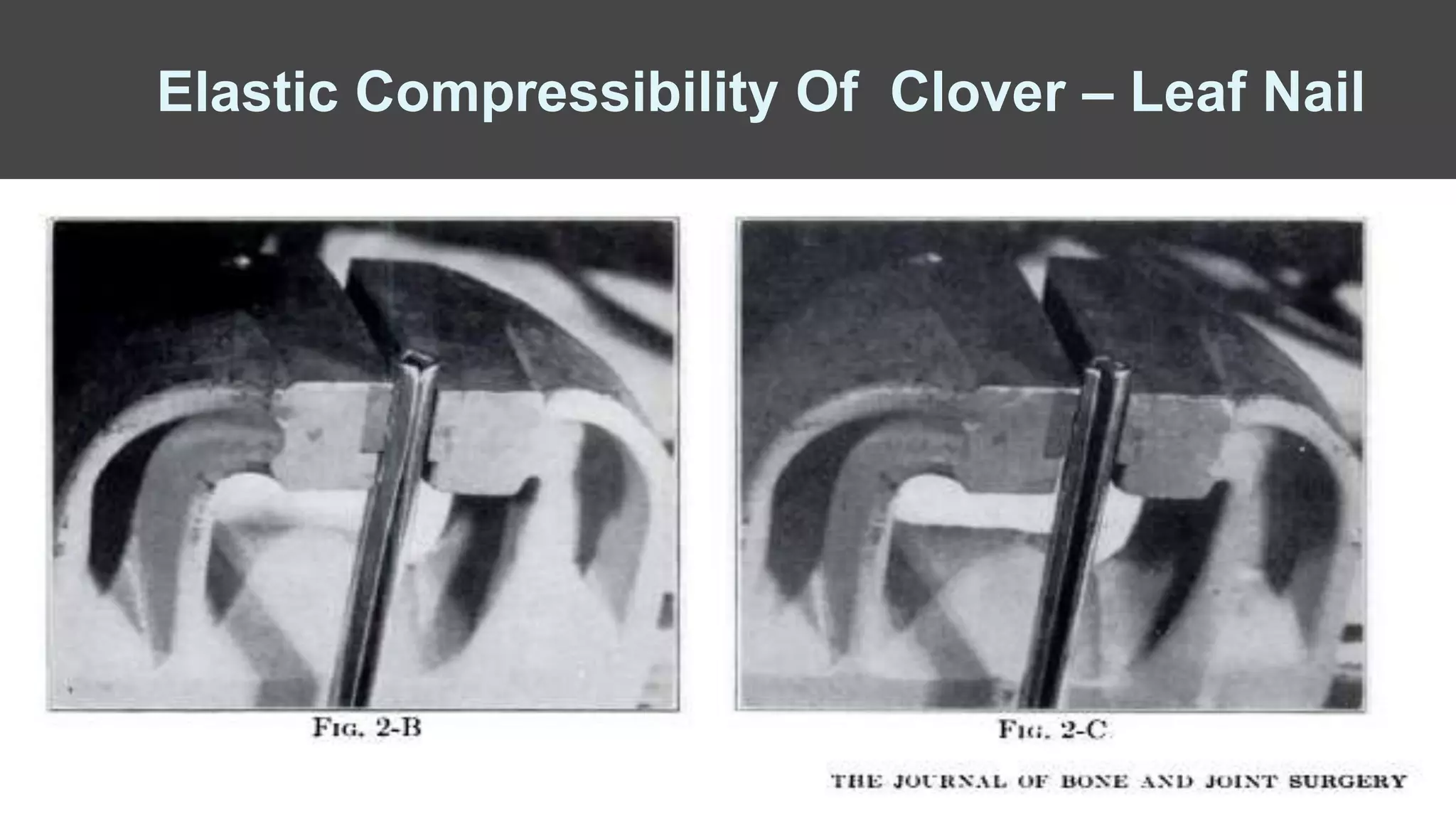
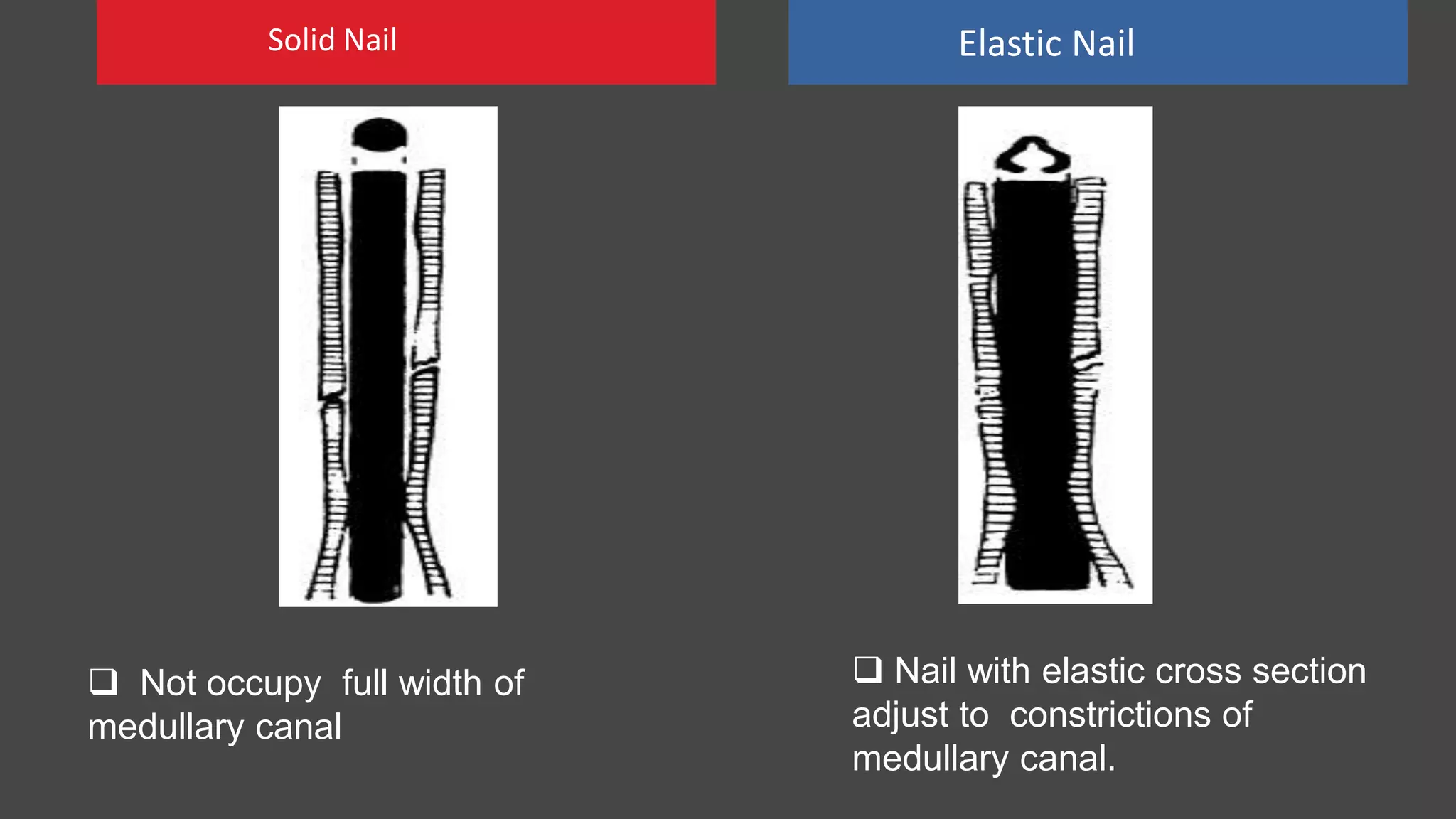
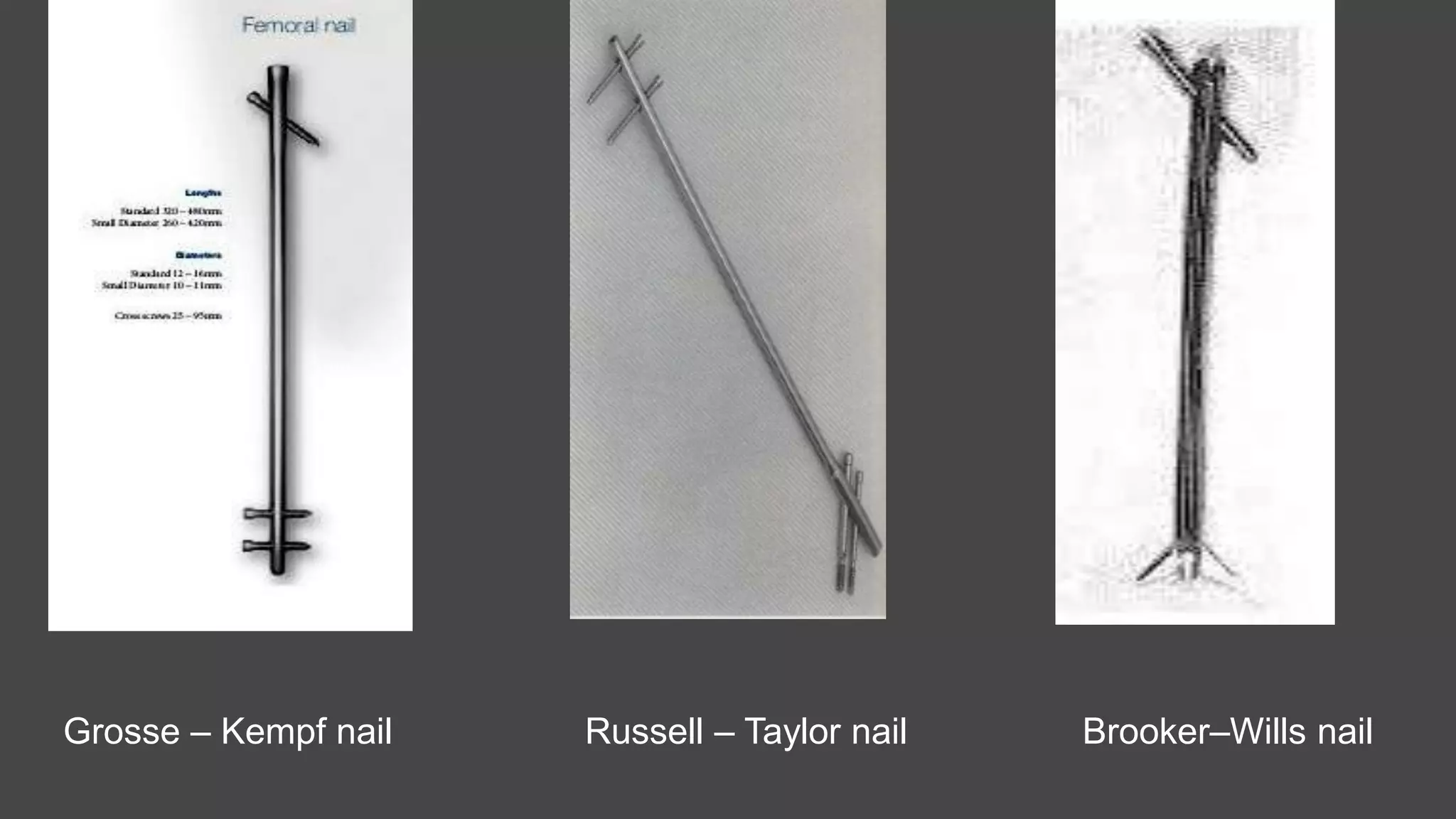
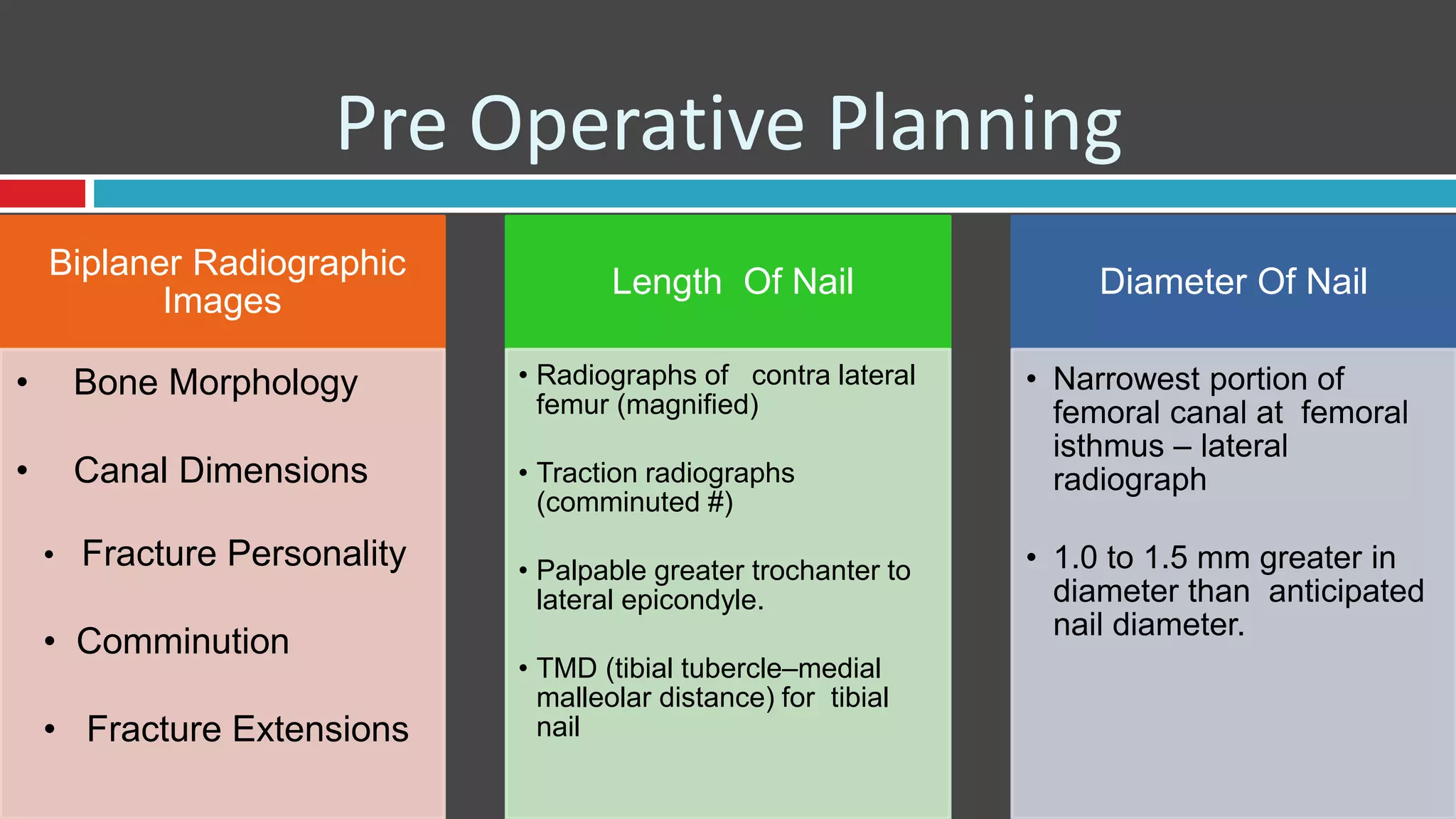
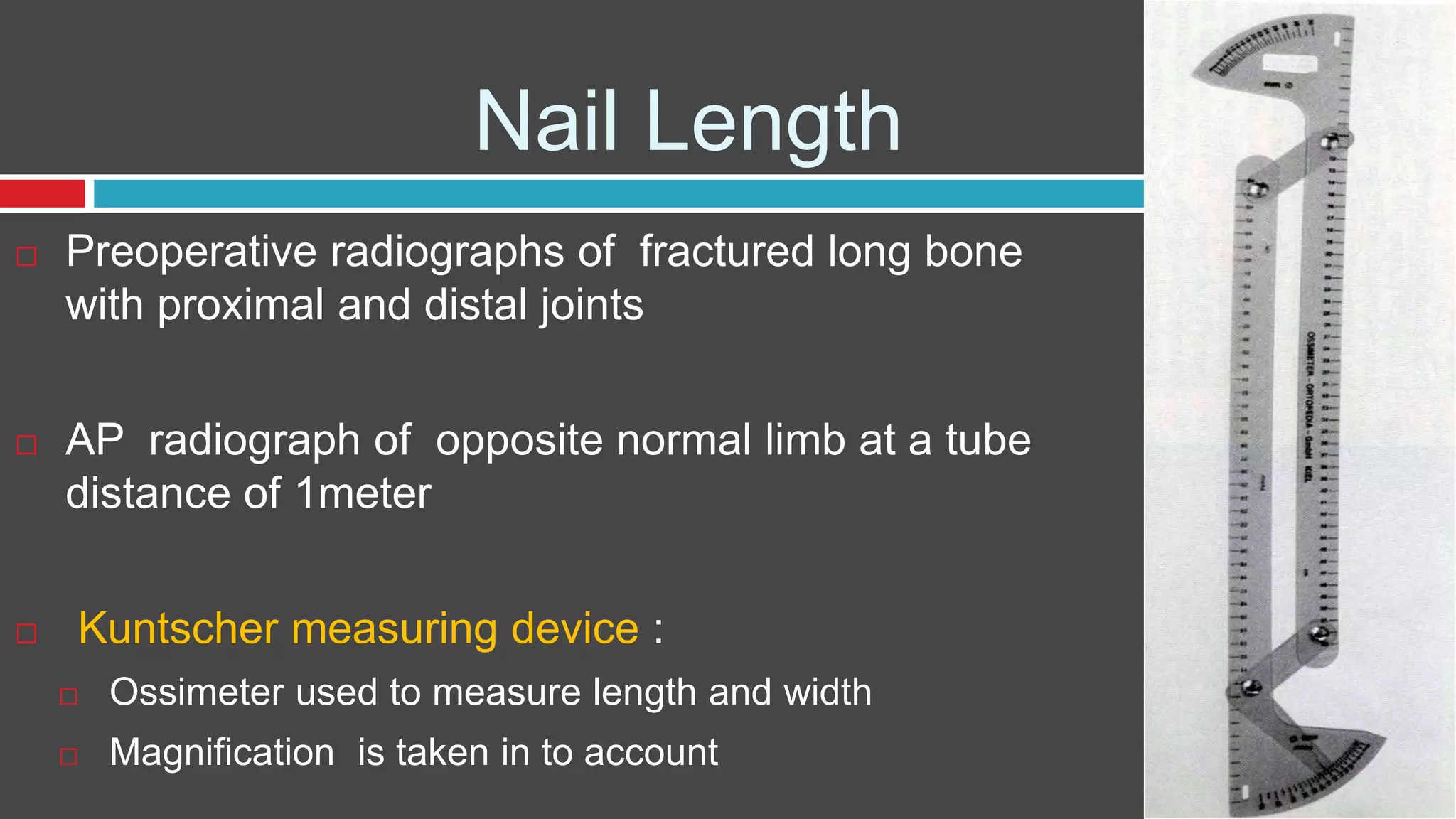
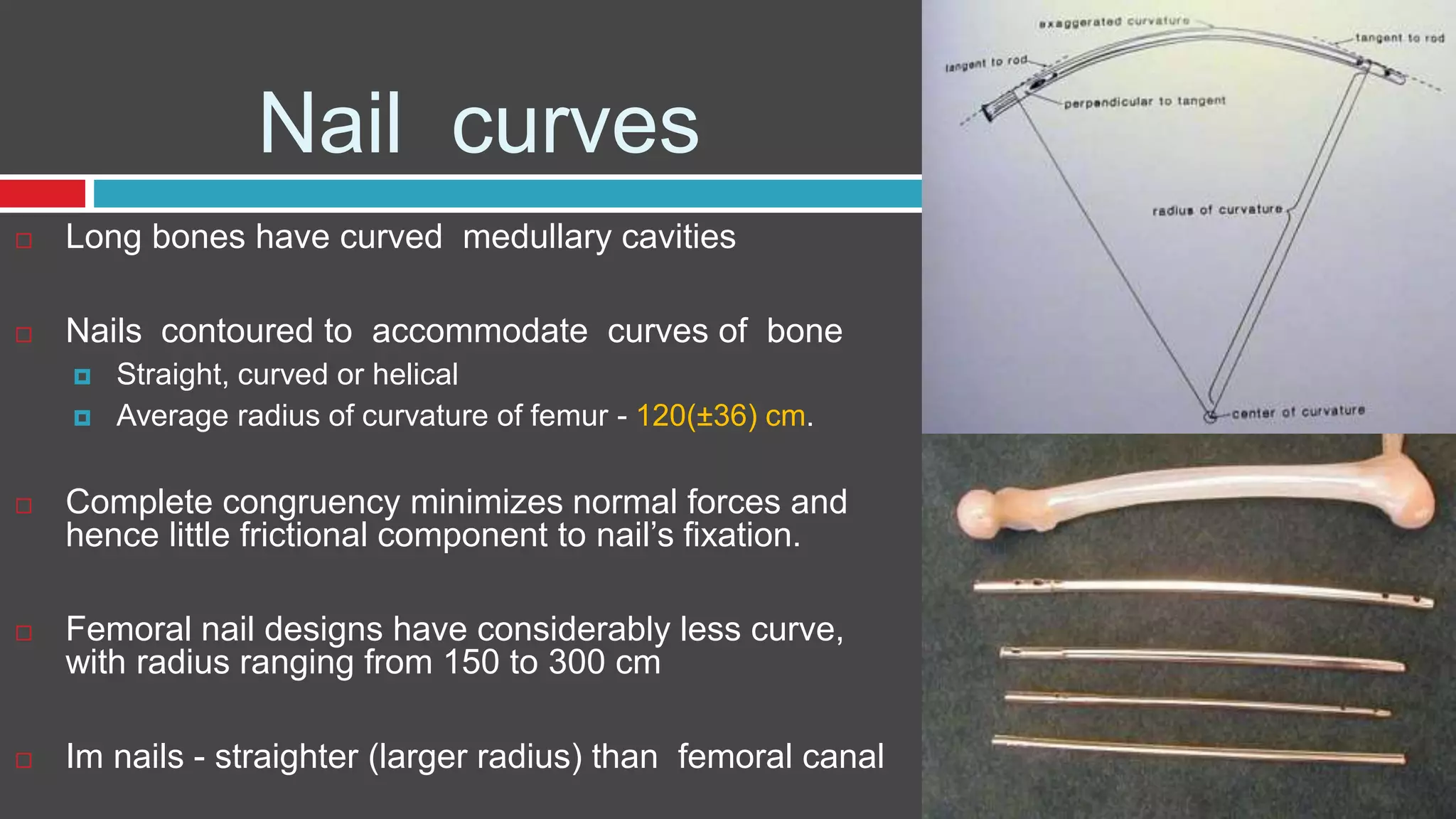
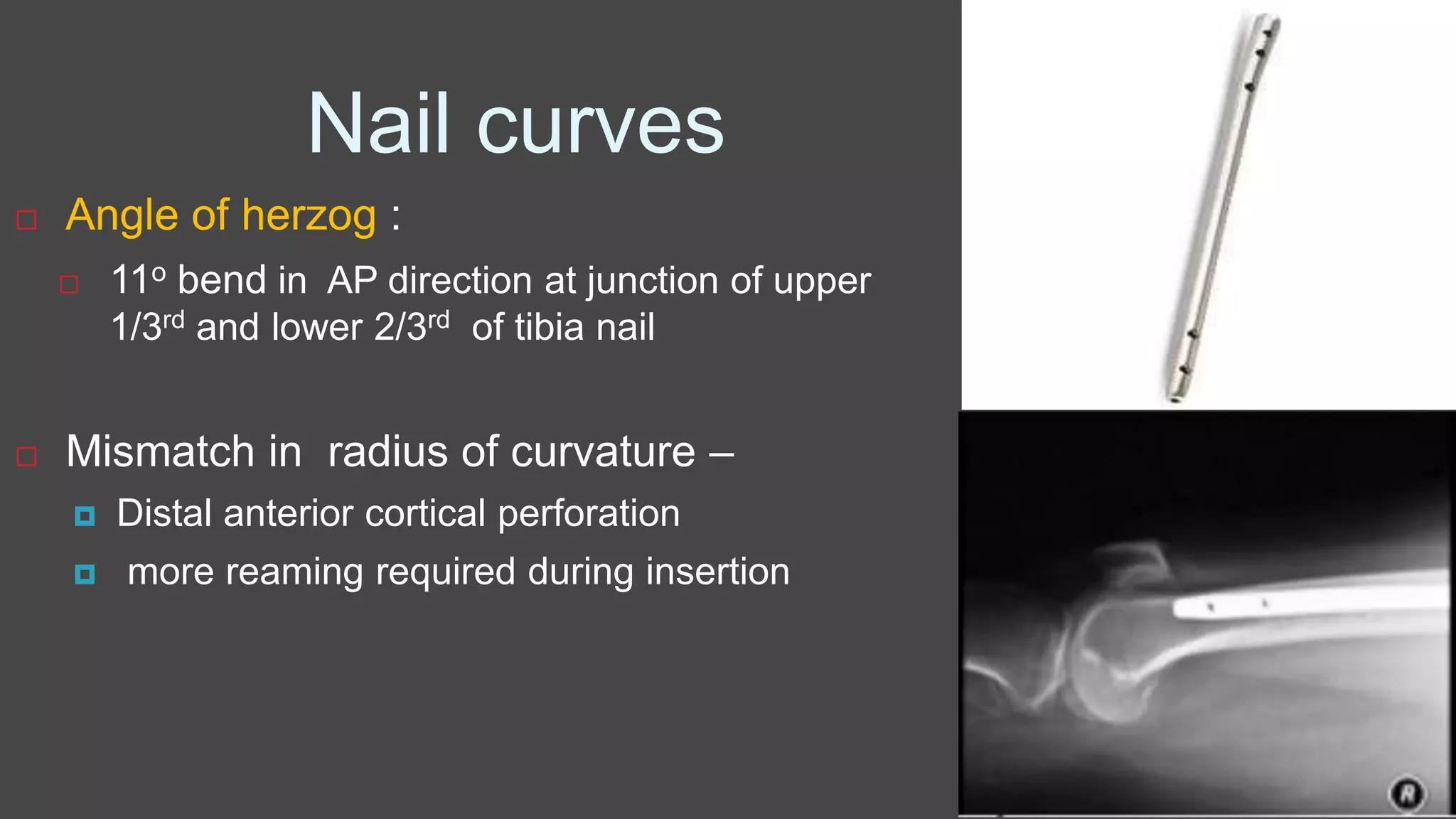
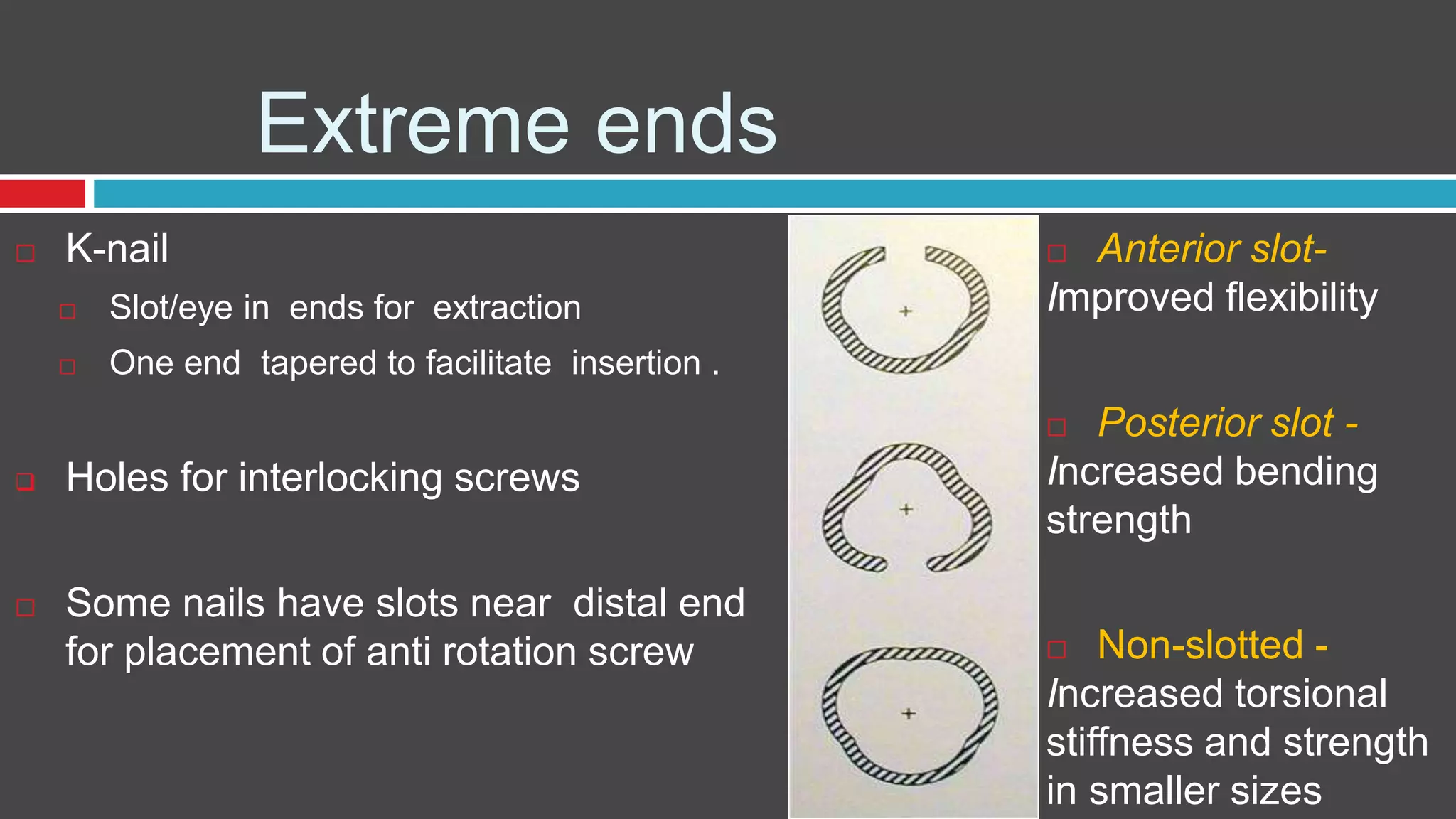
- Evolution from 1st to 3rd generation nails with improved stability and anatomical fit
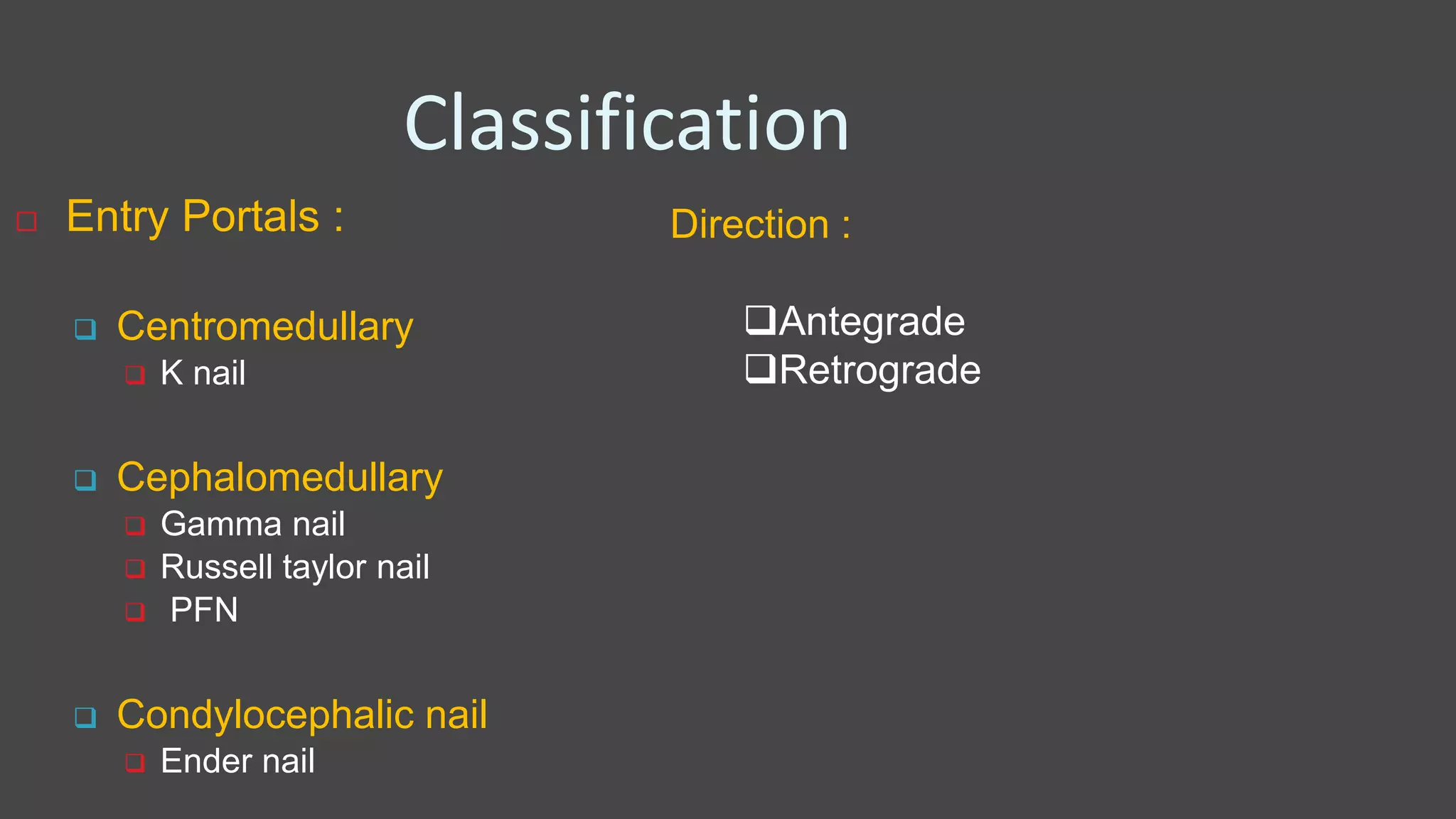
- Classification by entry point and direction of insertion
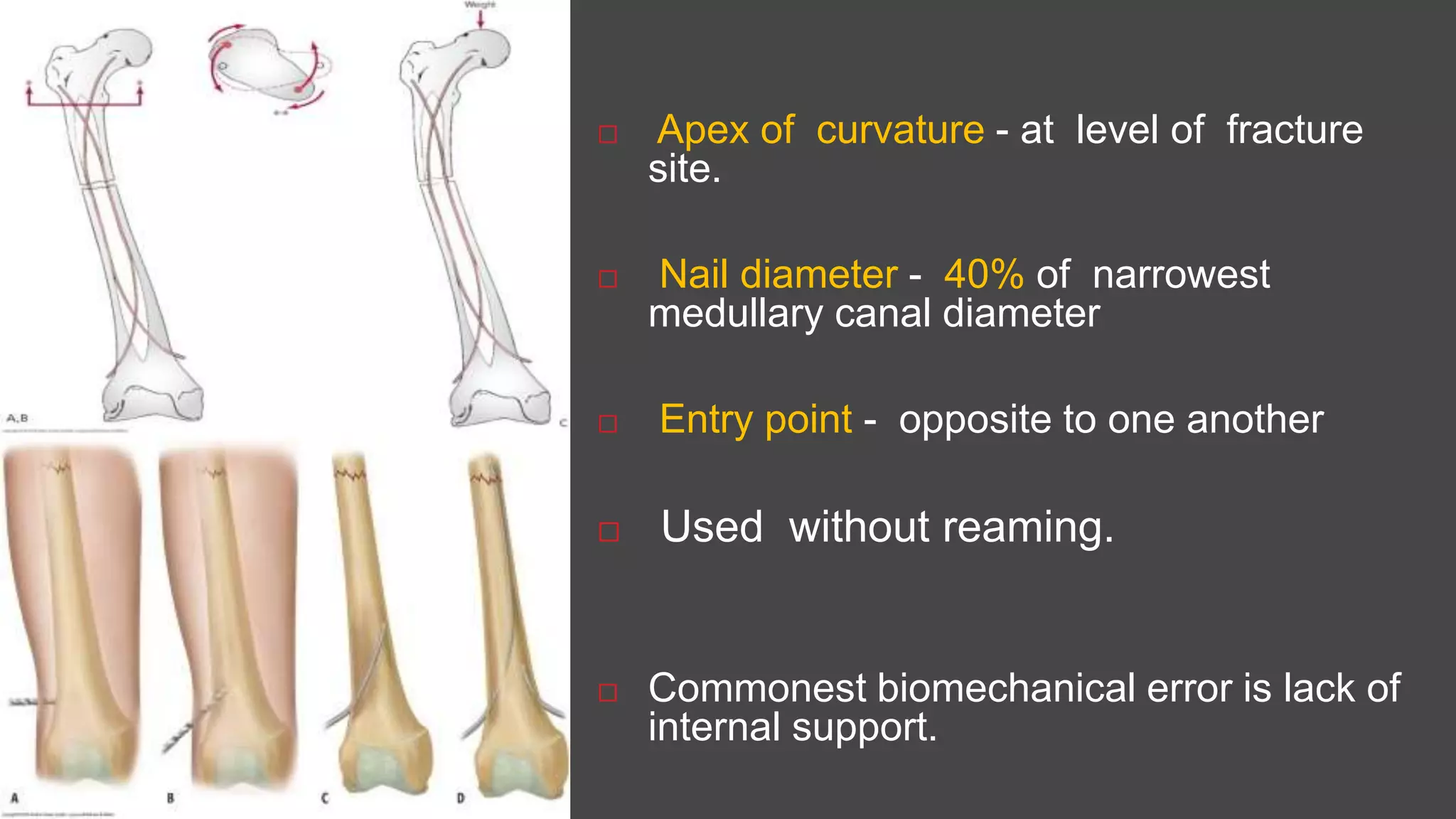
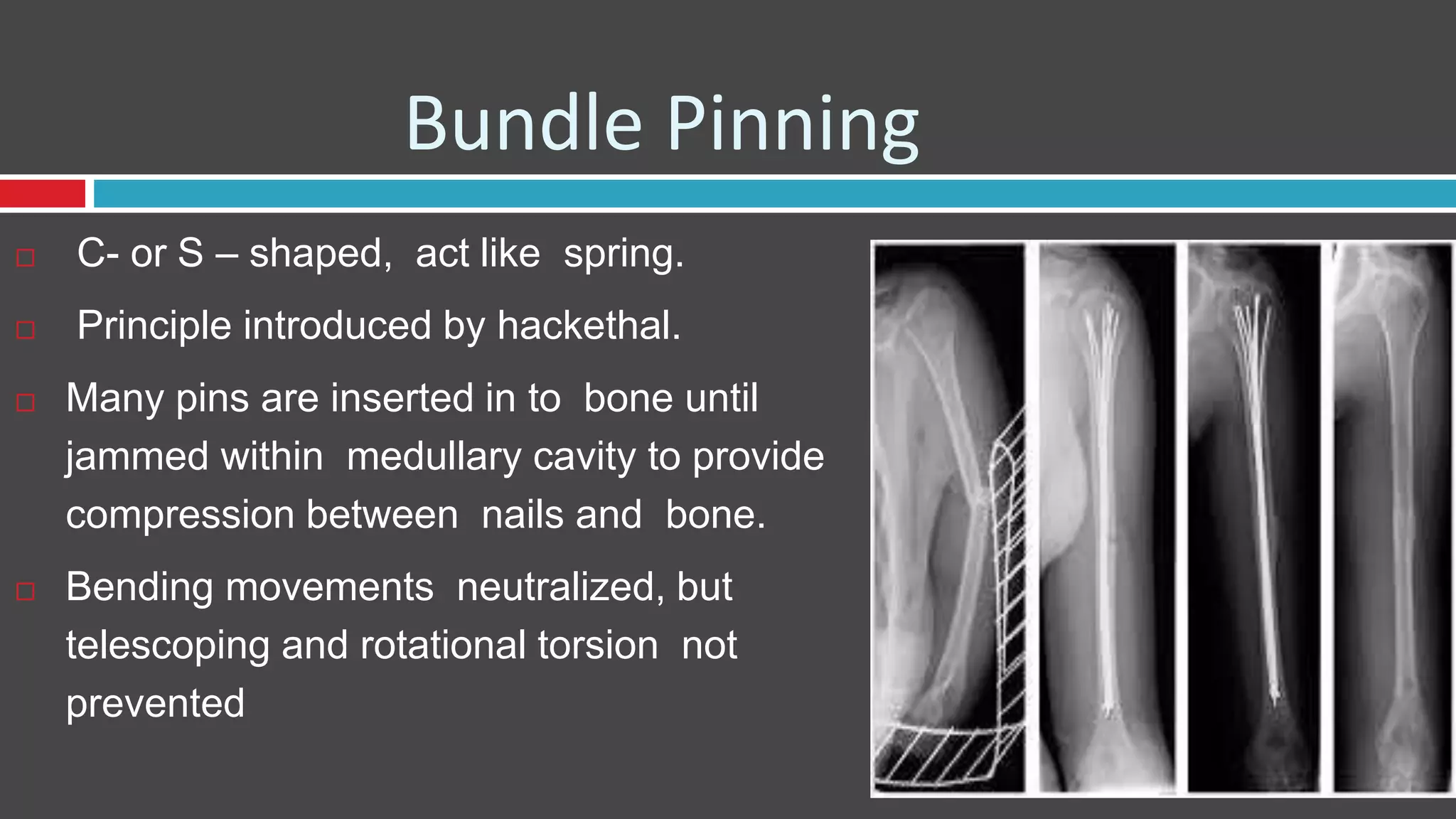
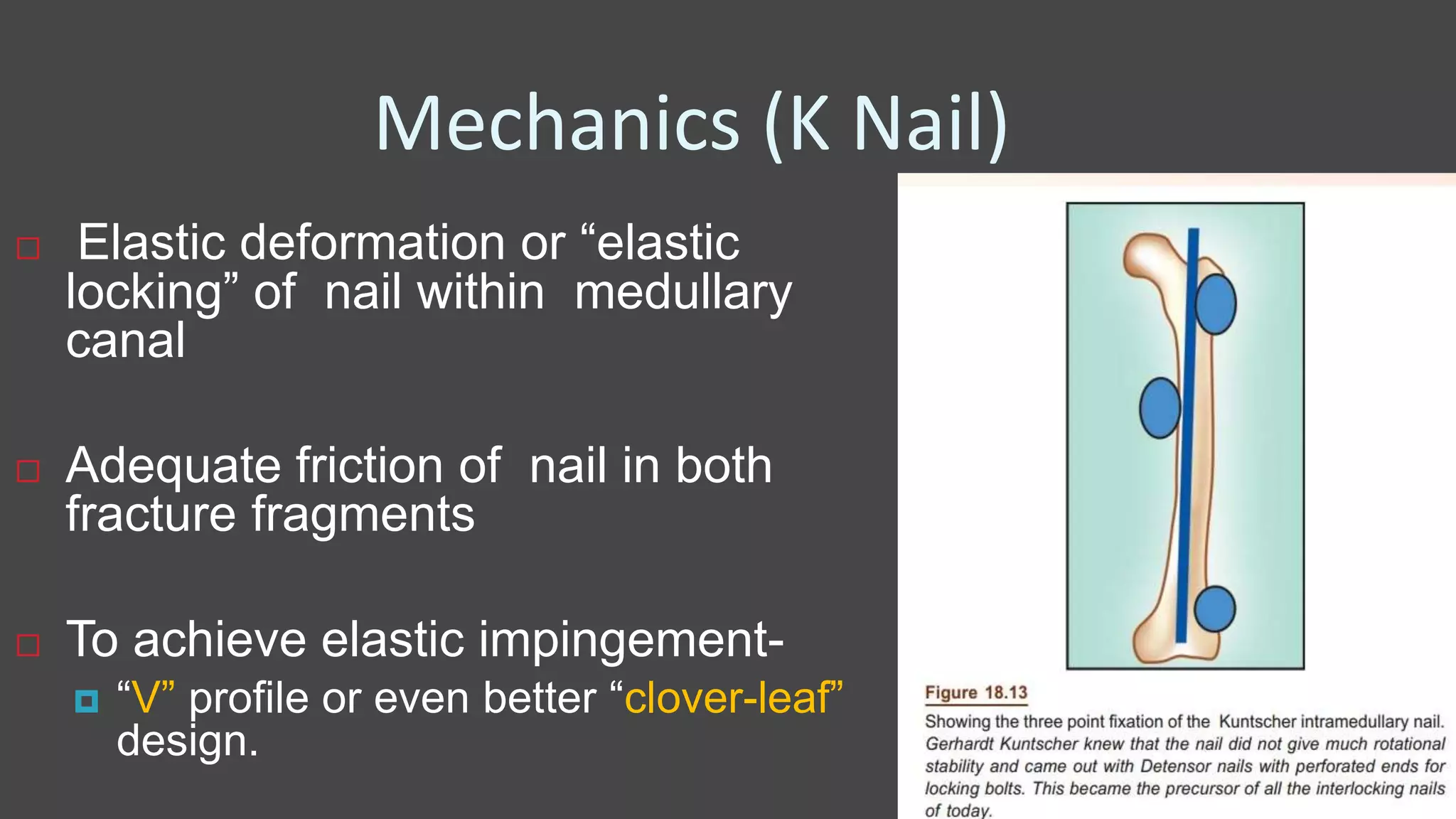
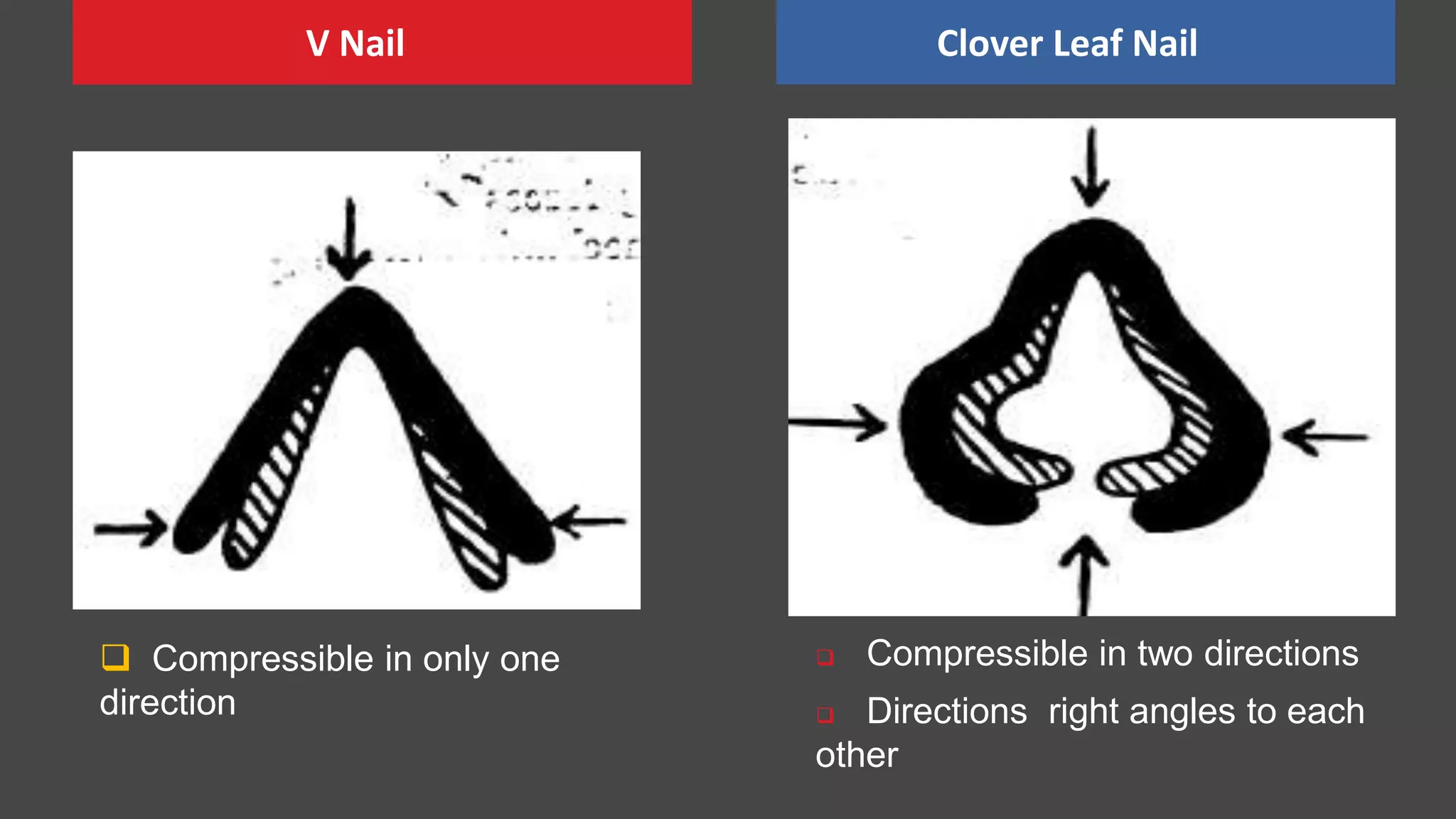
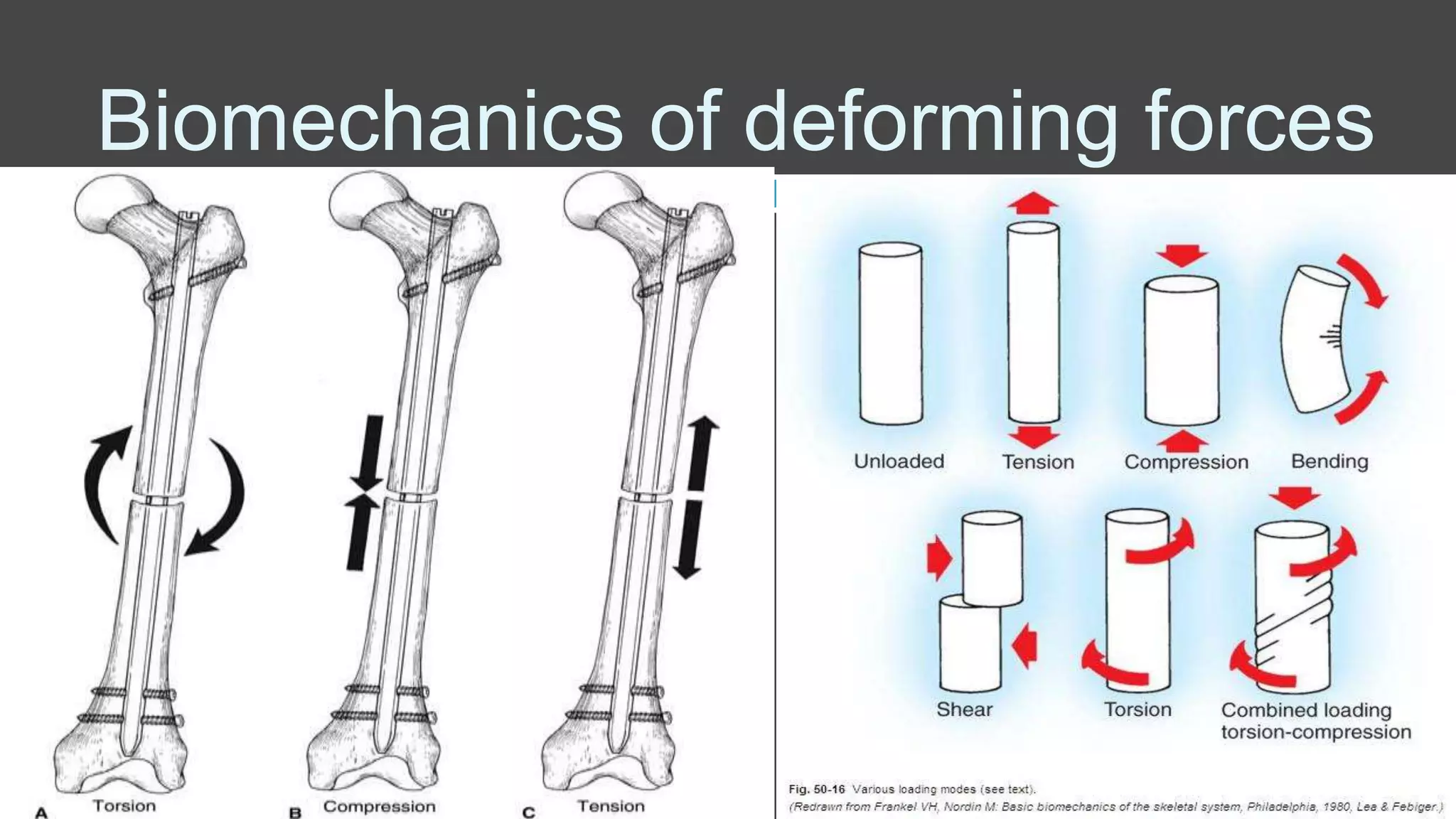
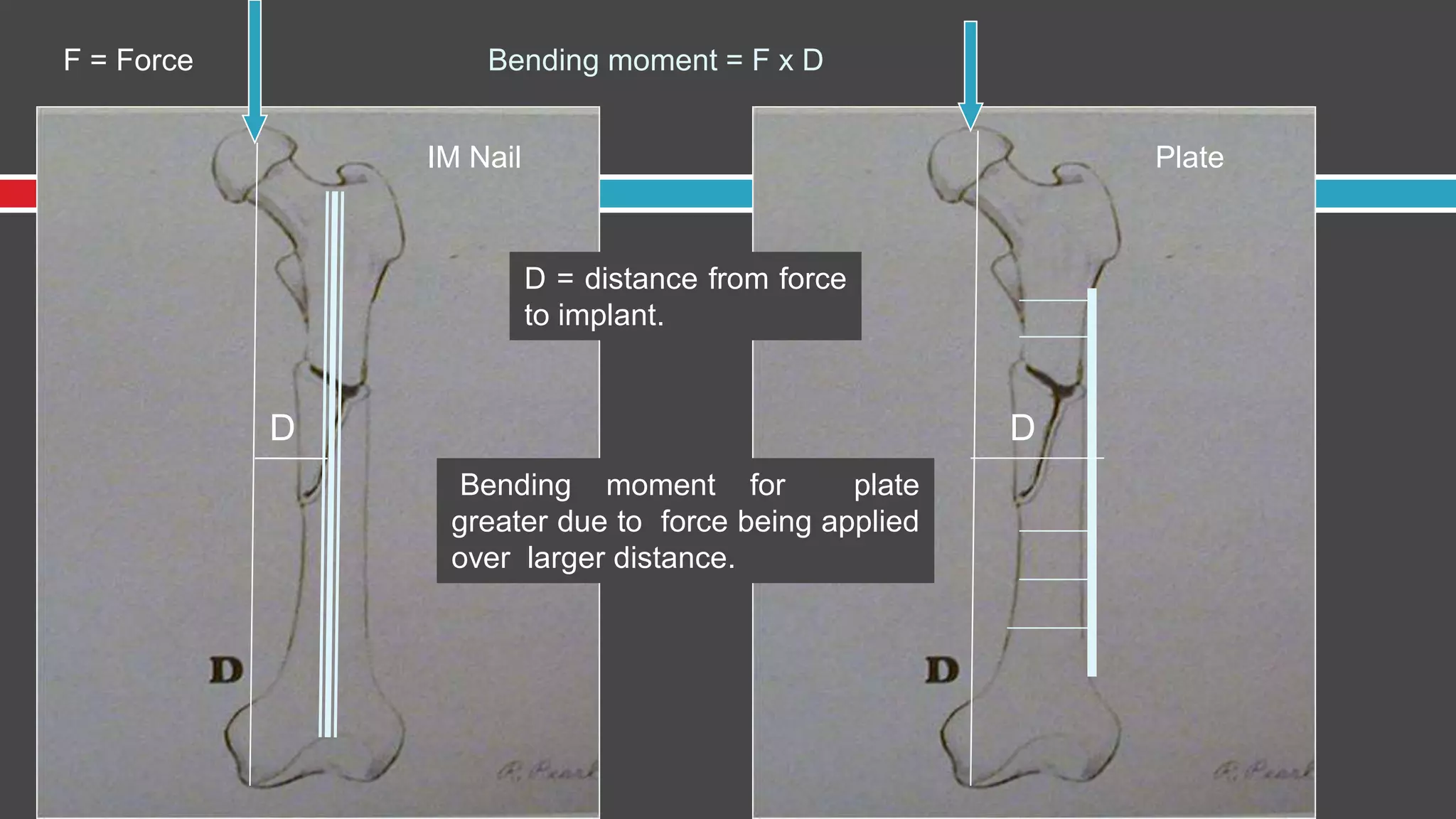
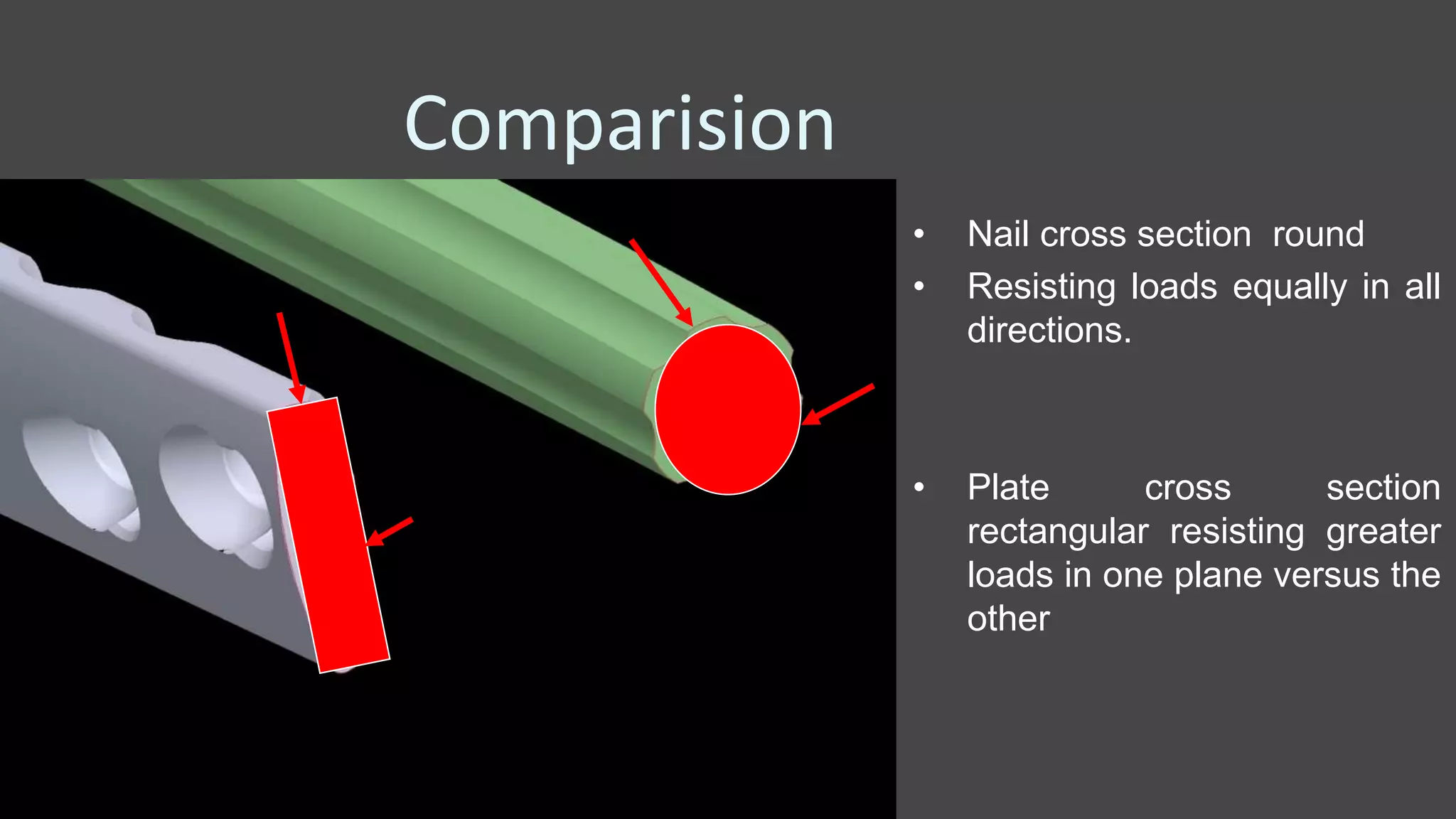
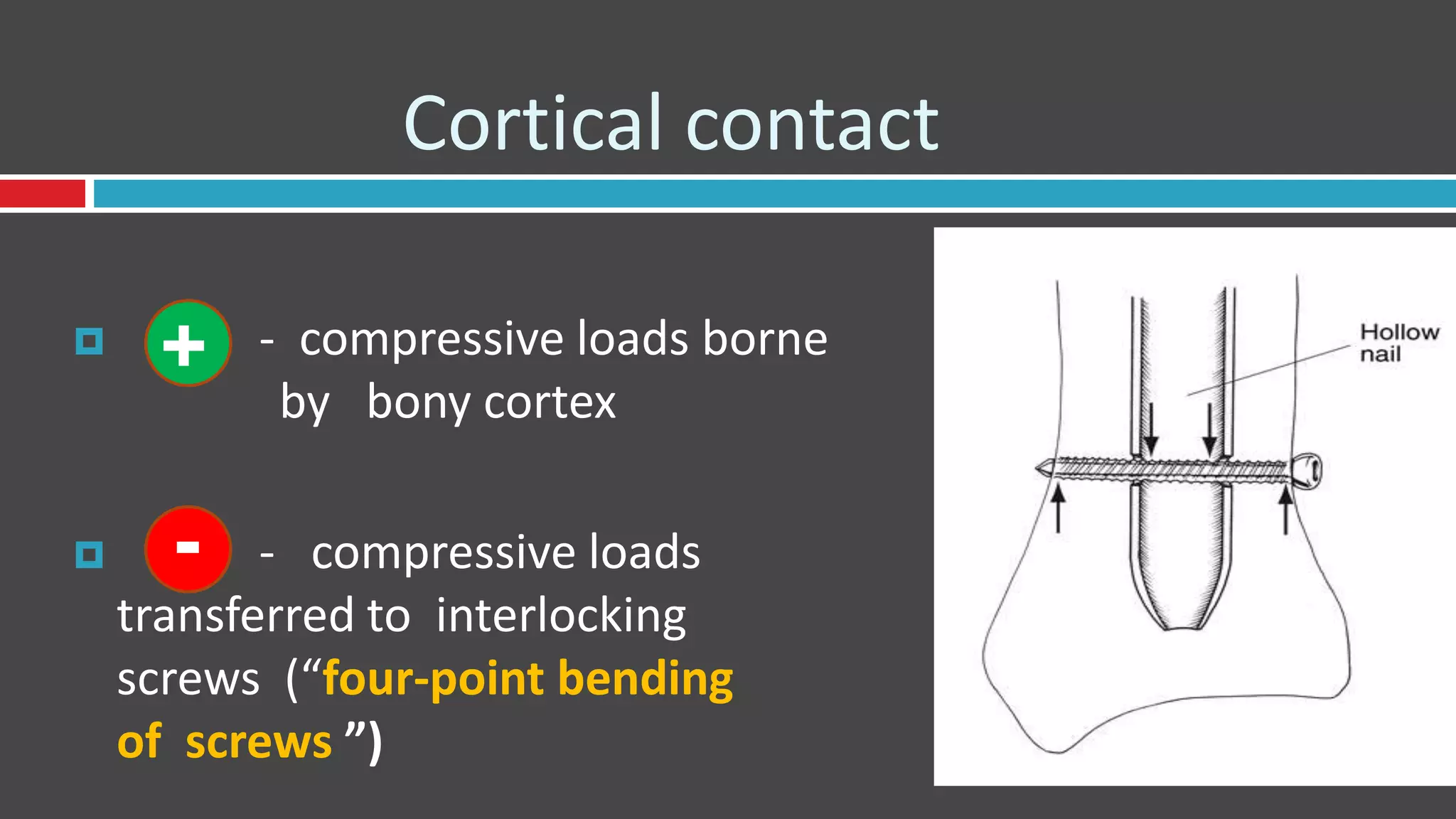
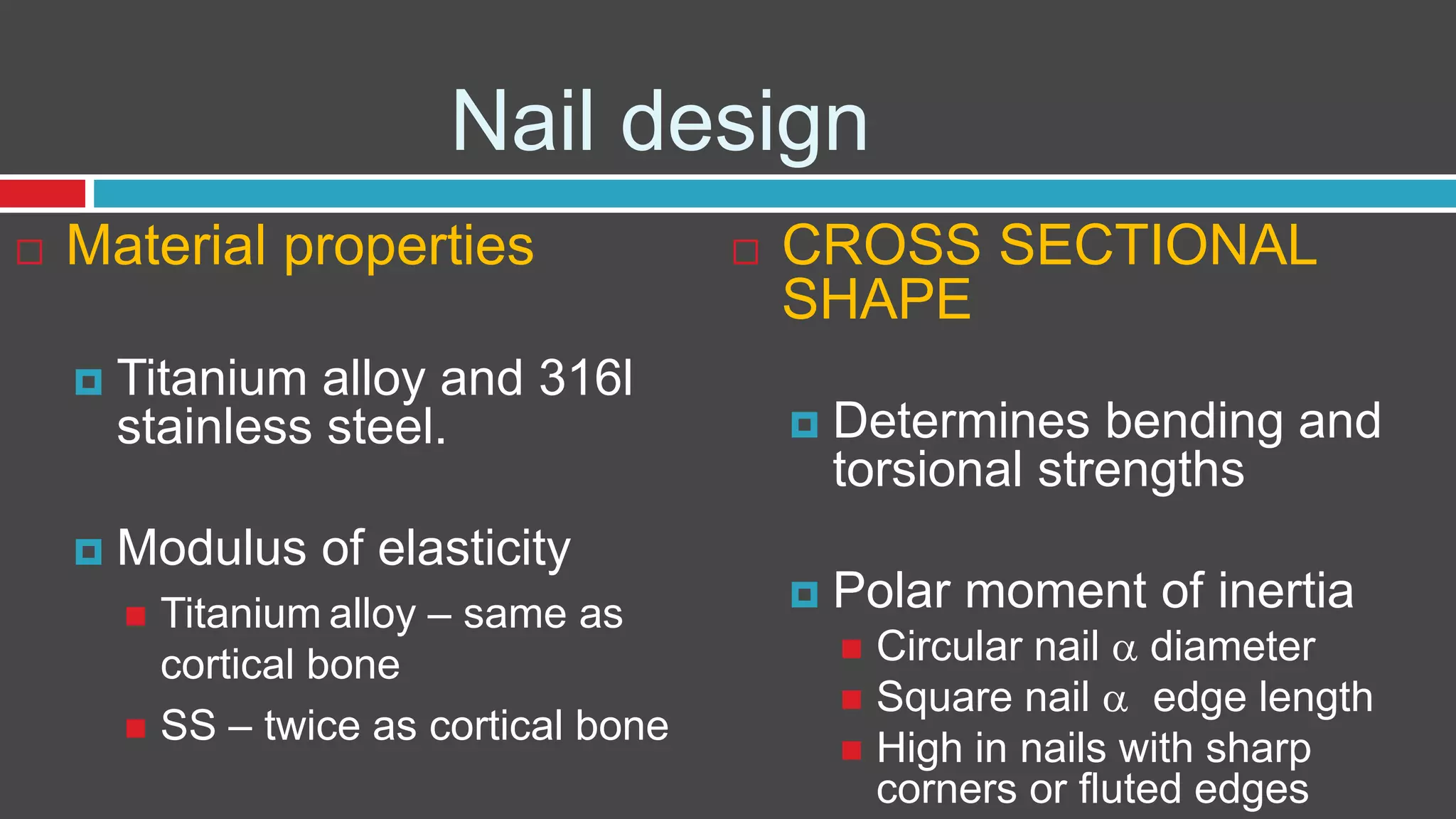
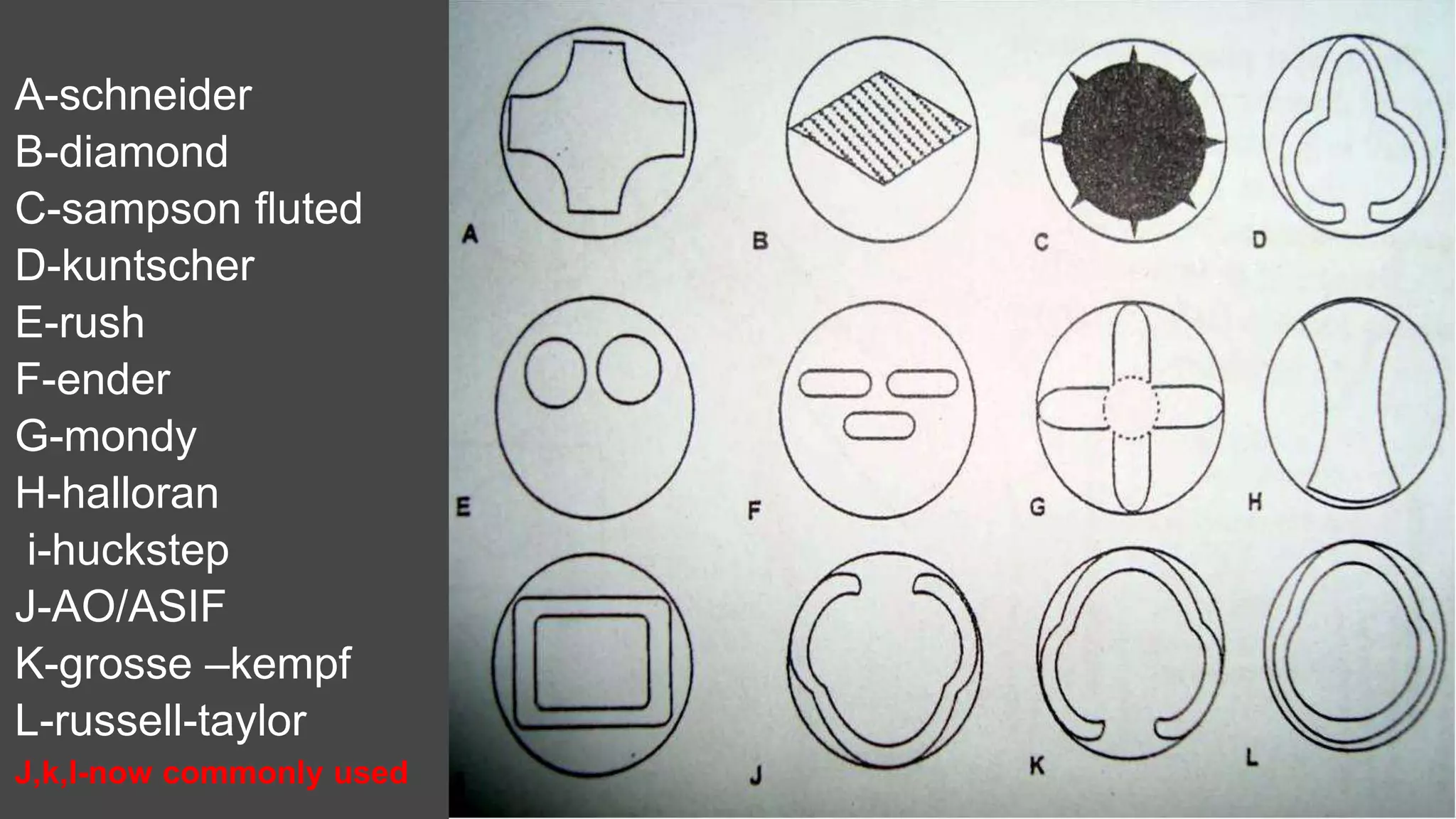
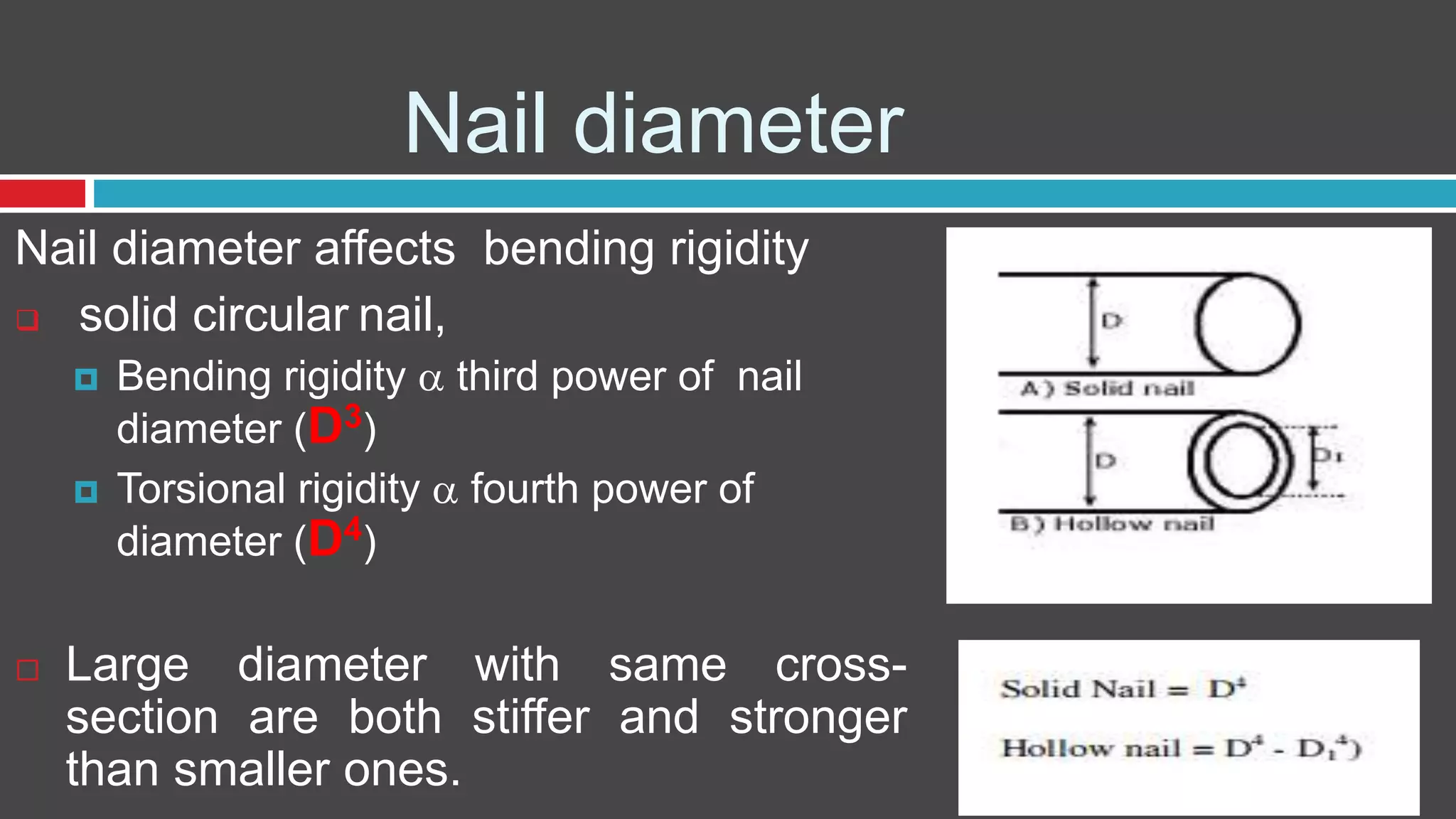
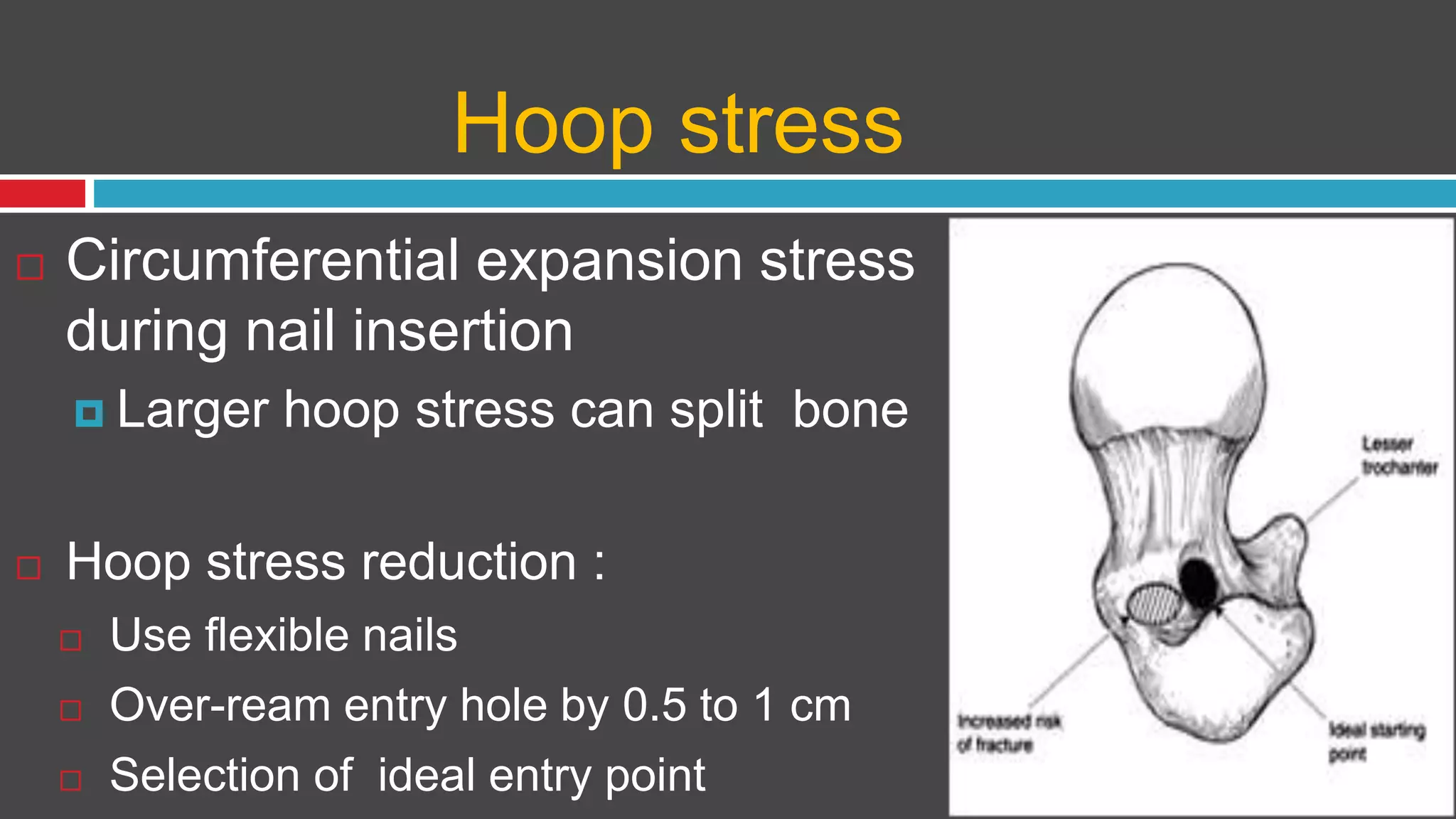
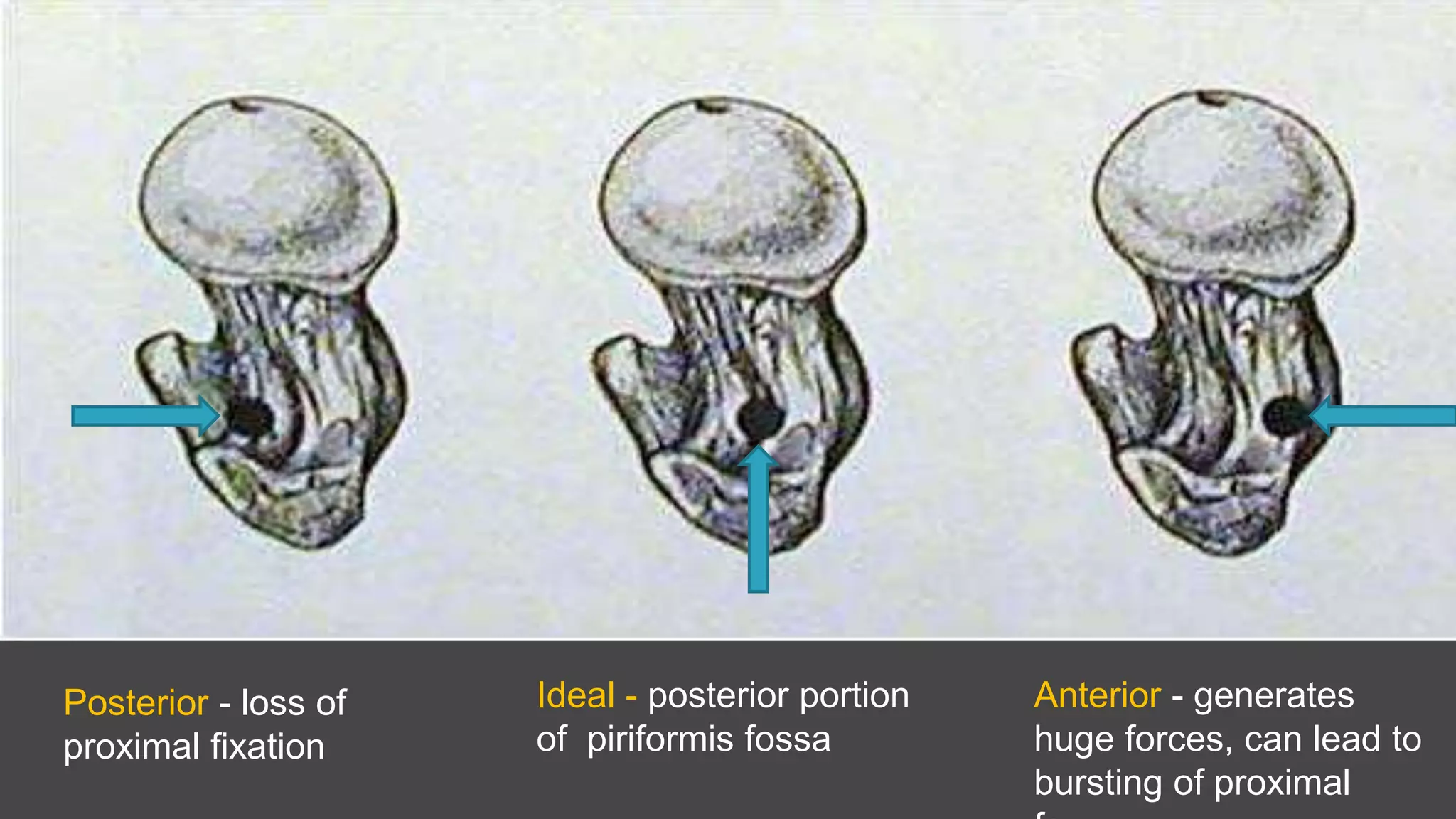
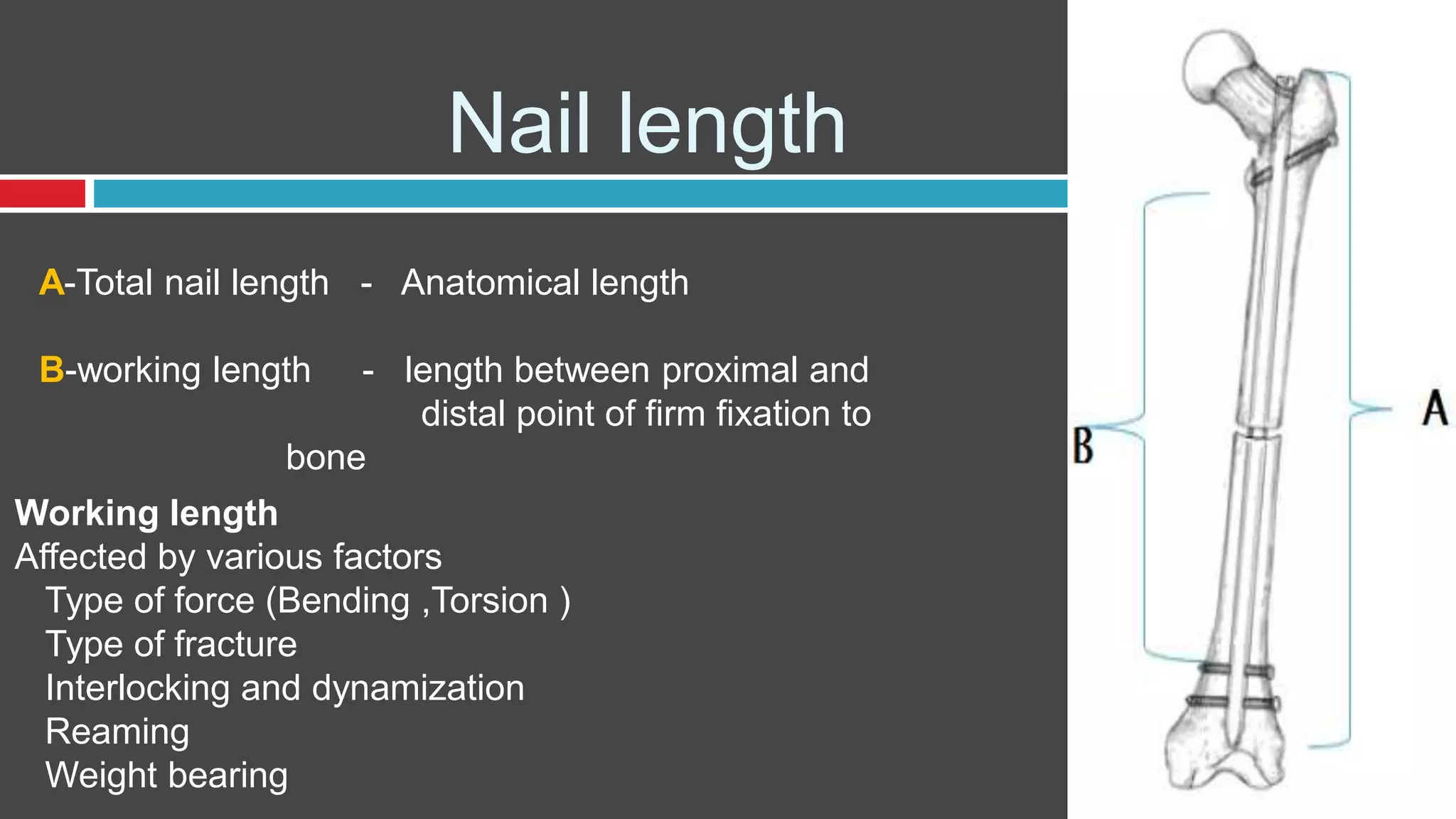
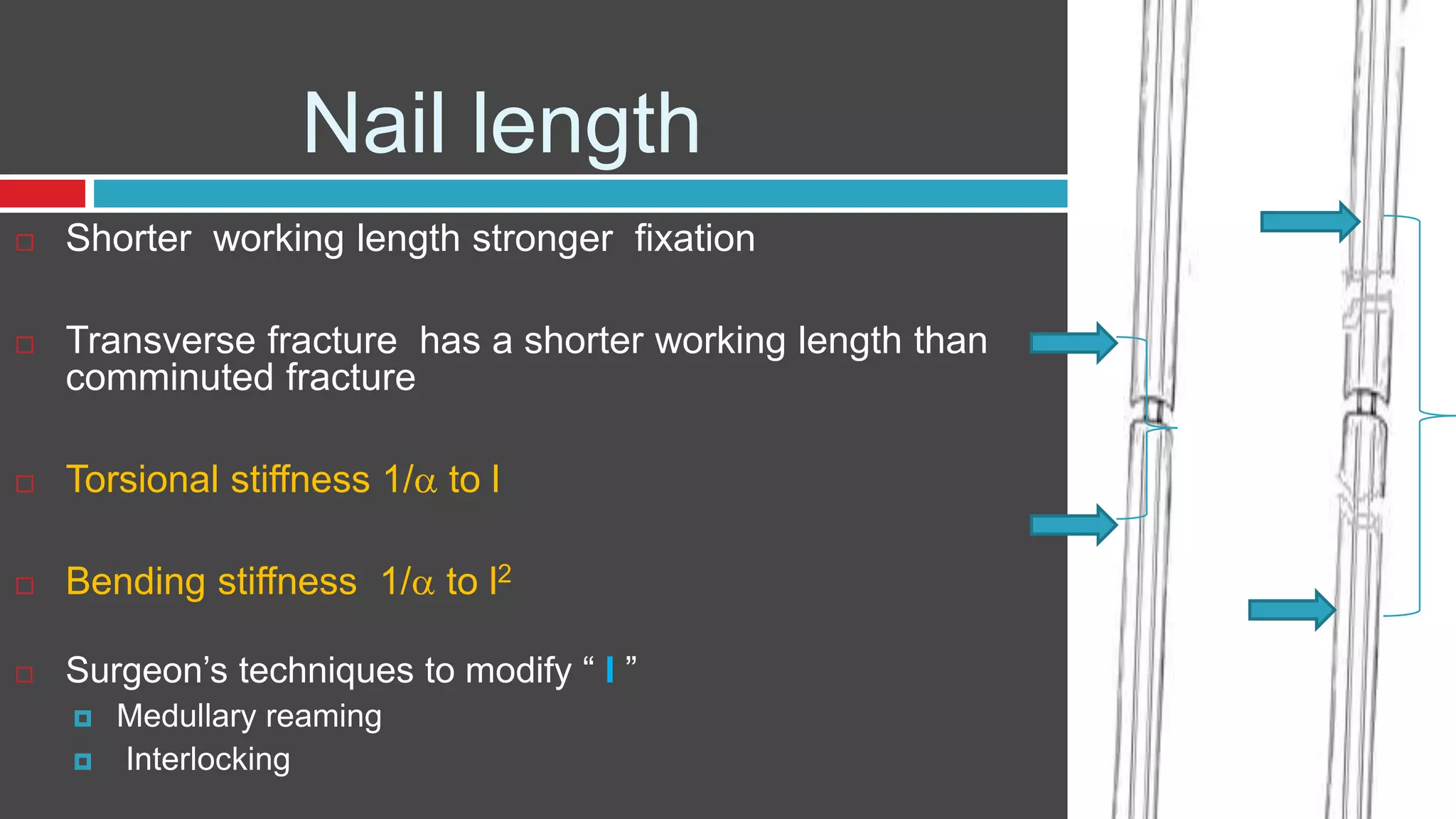
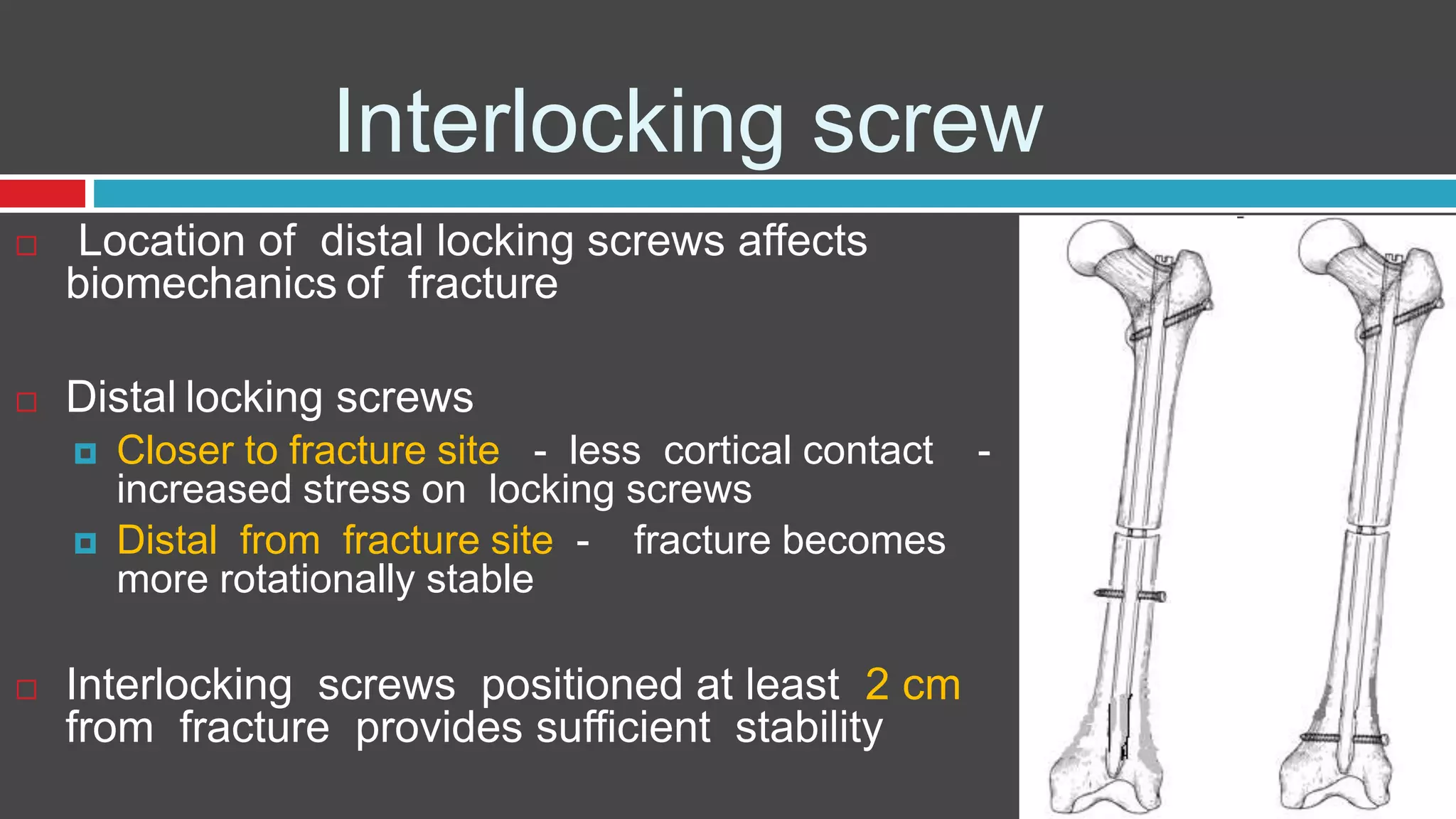
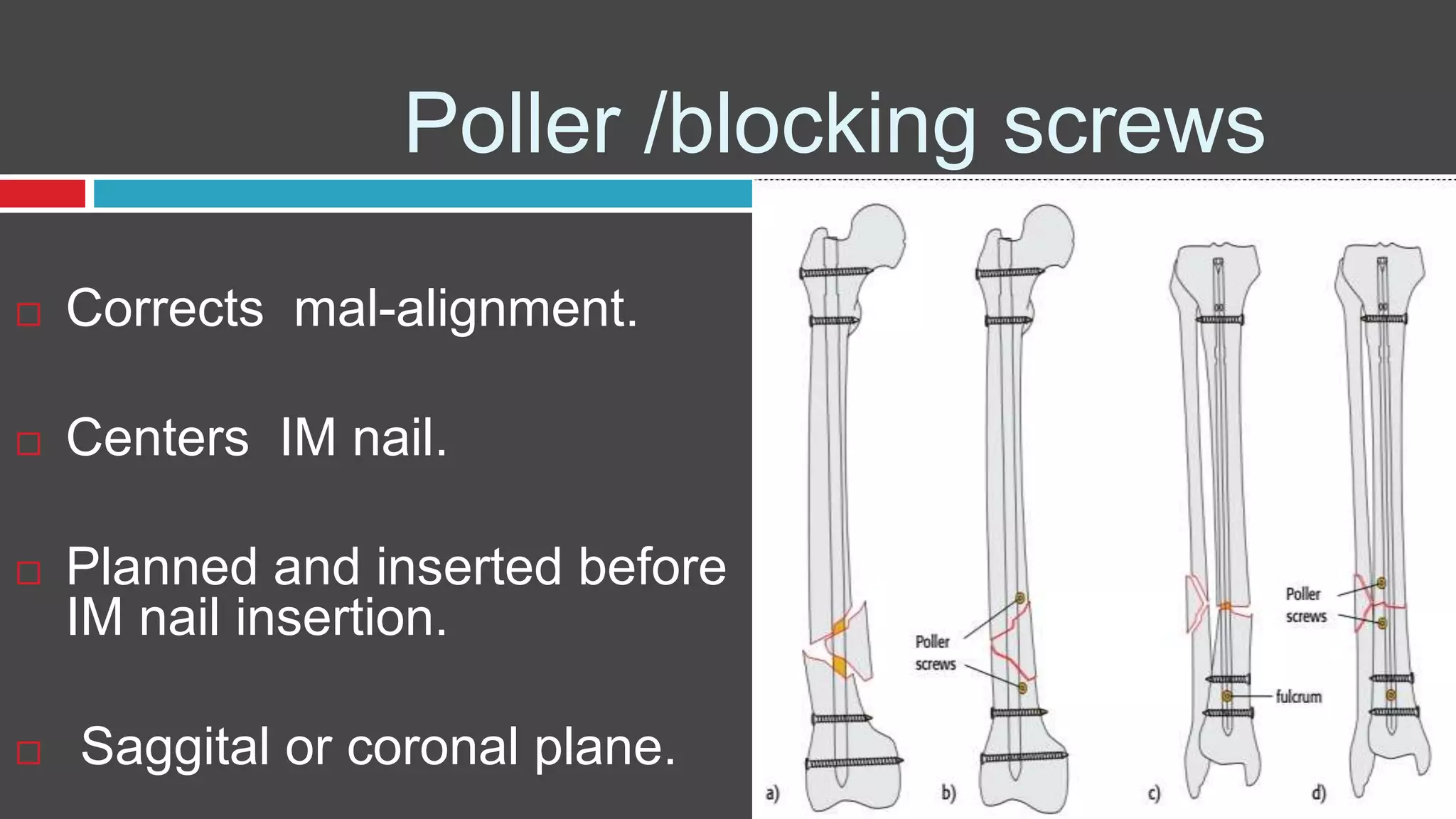
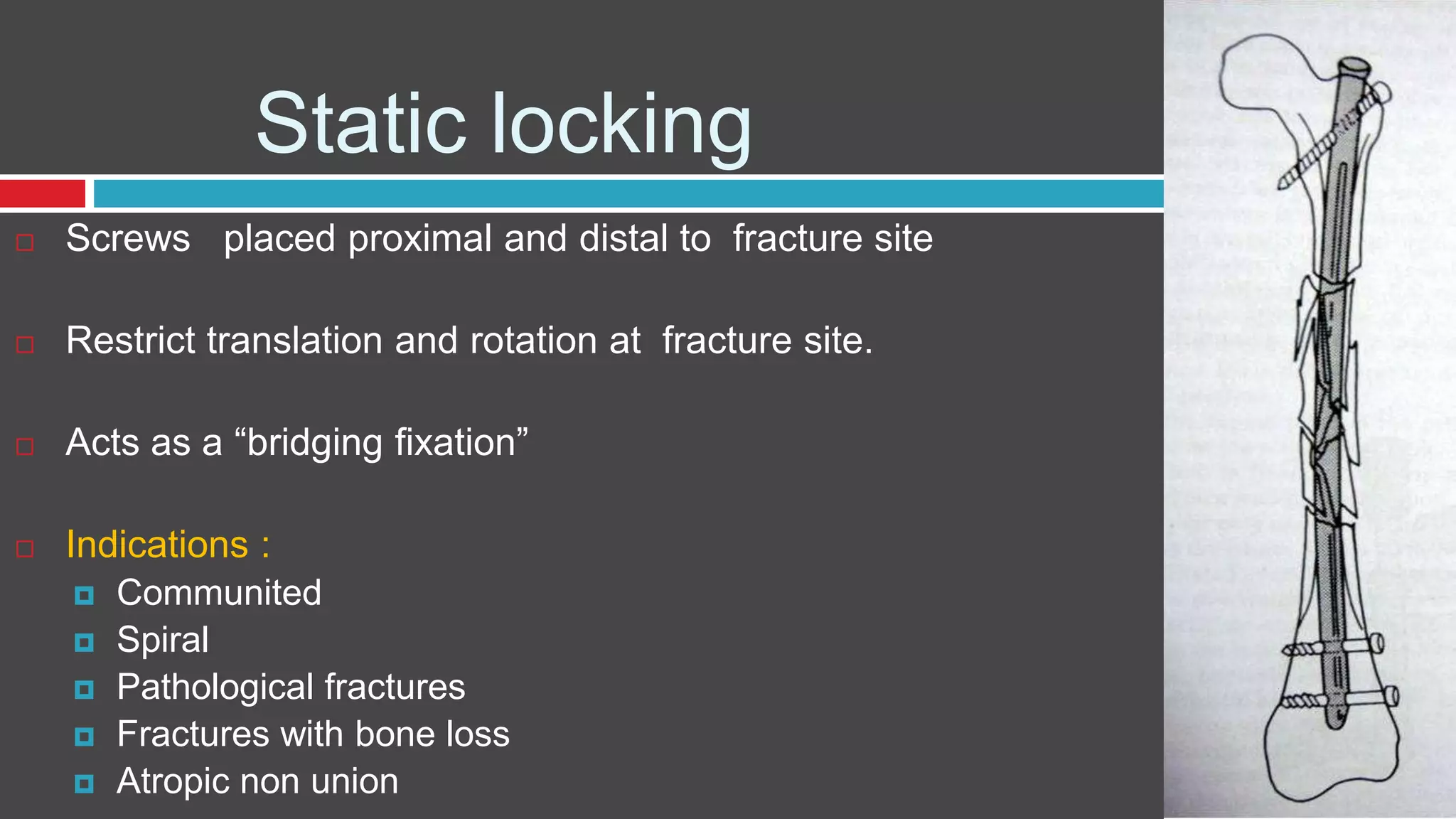
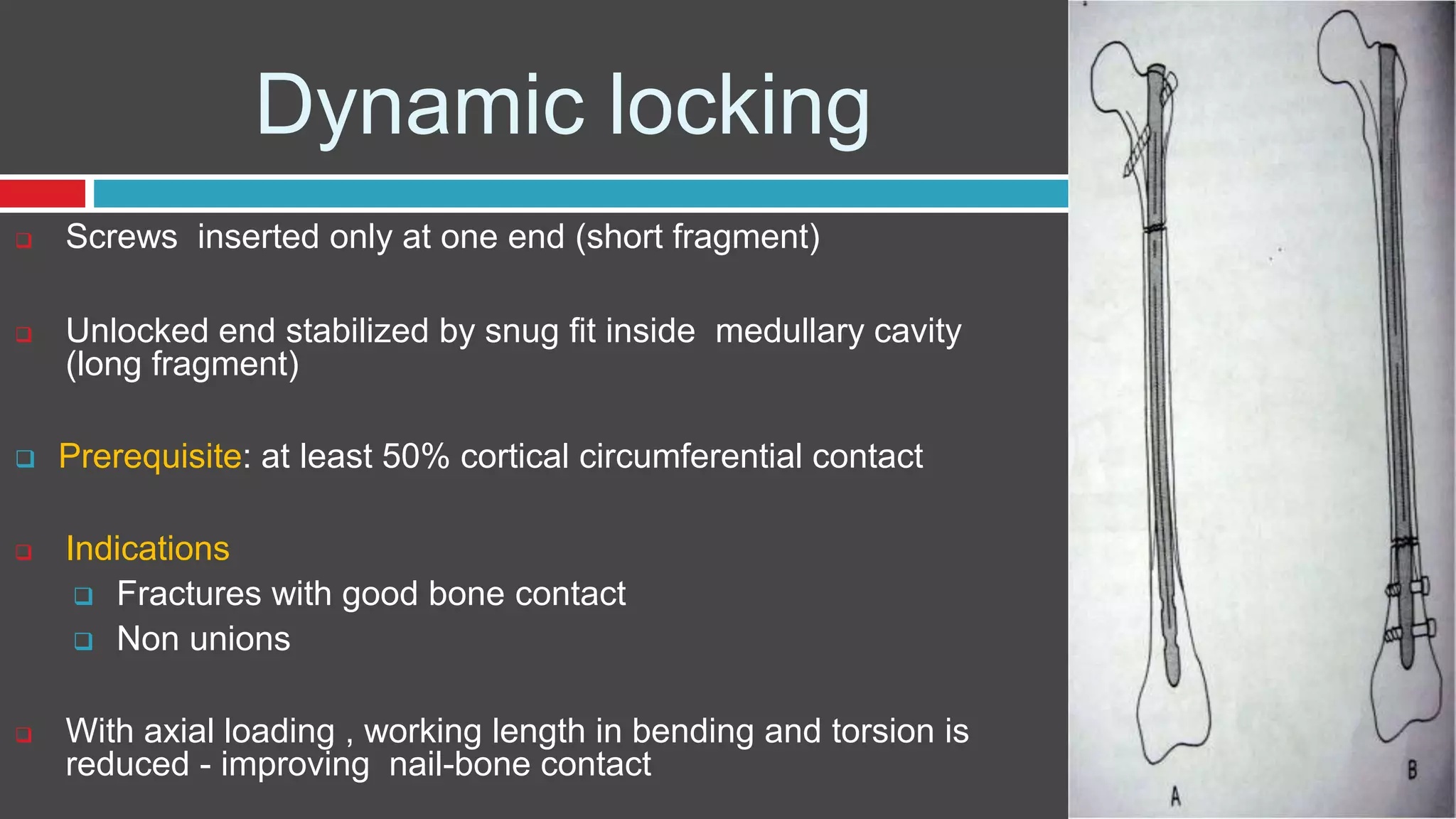
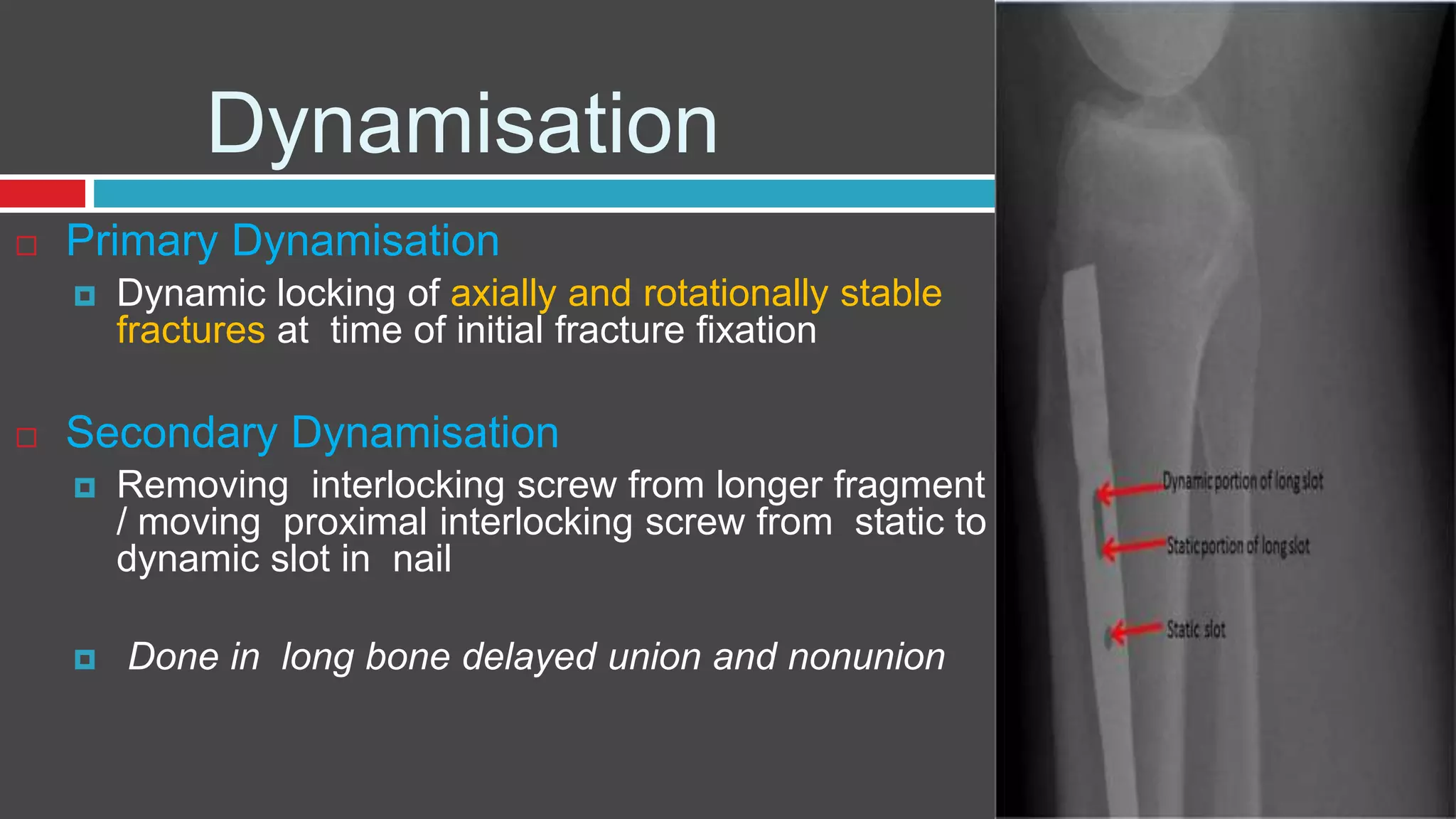
- Biomechanical principles of load transfer and stability depending on nail design, number/location of locking screws, and reaming
- Applications for treating fractures of long bones and considerations for special circumstances