This document provides a summary of the temporomandibular joint (TMJ) and temporomandibular joint disorders (TMD) in 3 paragraphs:
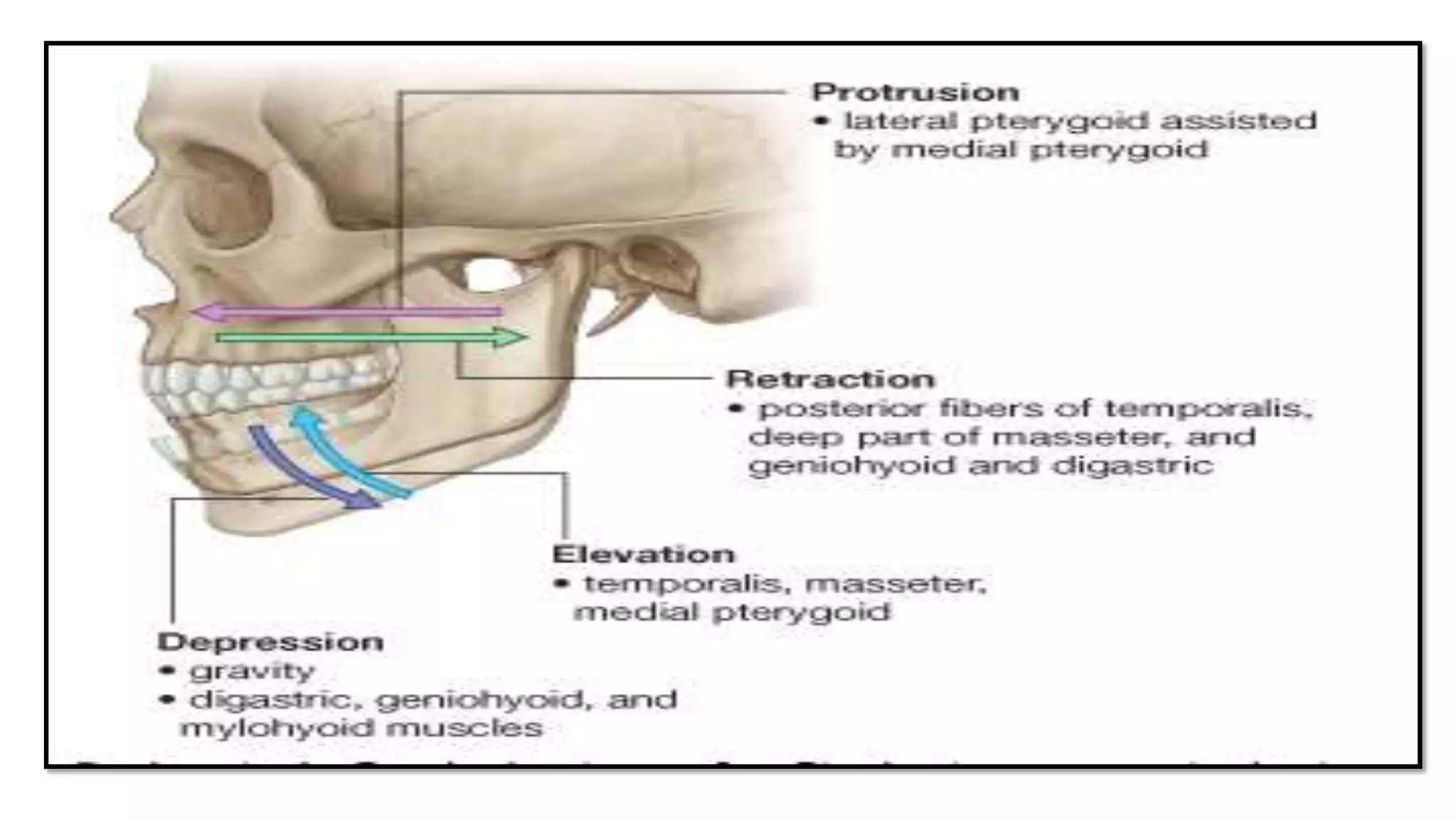
The first paragraph describes the anatomy of the TMJ, including its components like the glenoid fossa, articular eminence, condyle, separating disc, joint capsule, and ligaments. It also discusses the articulatory system involving the TMJ, muscles of mastication, occlusion of teeth, and nerve supply.
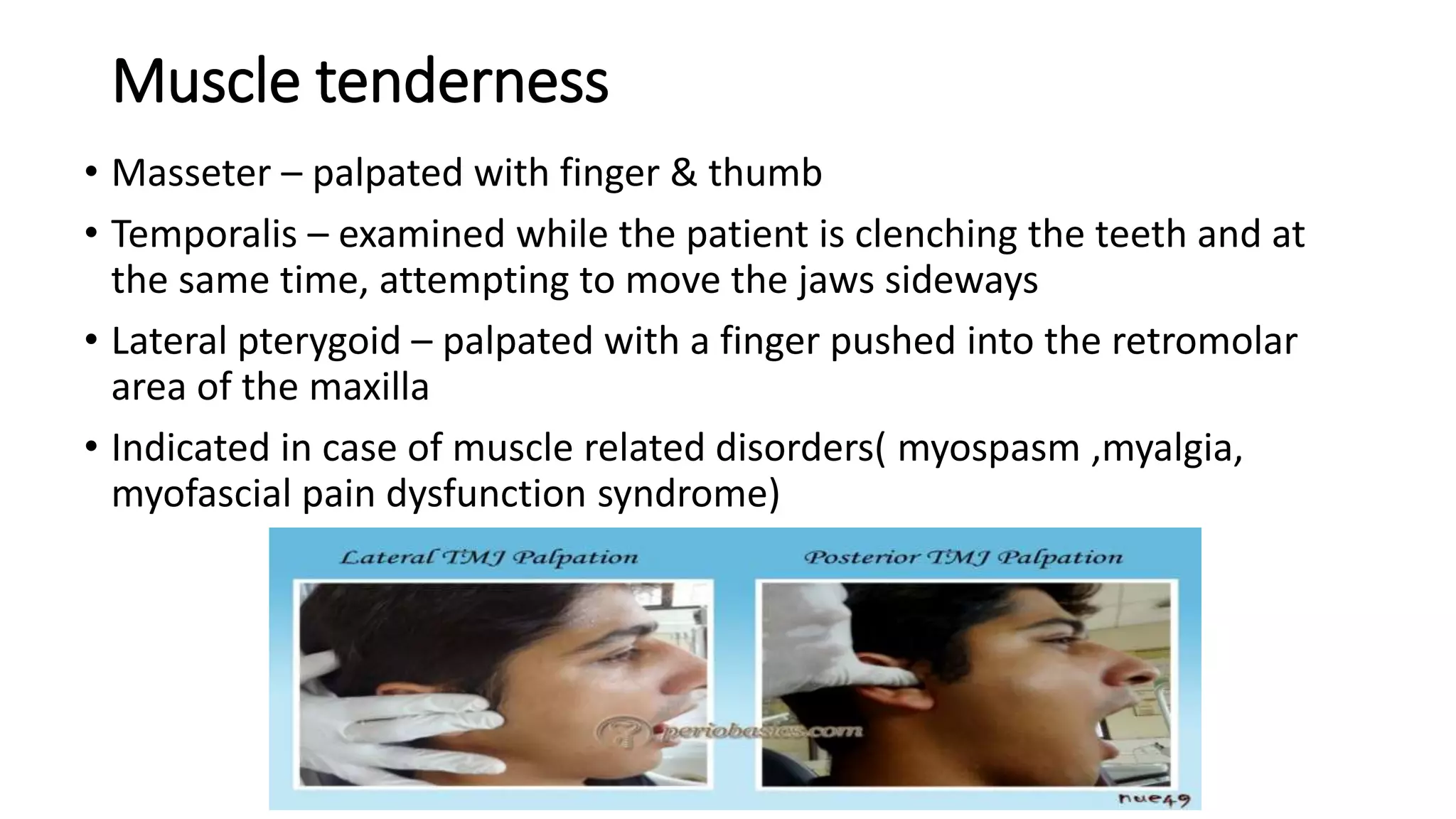
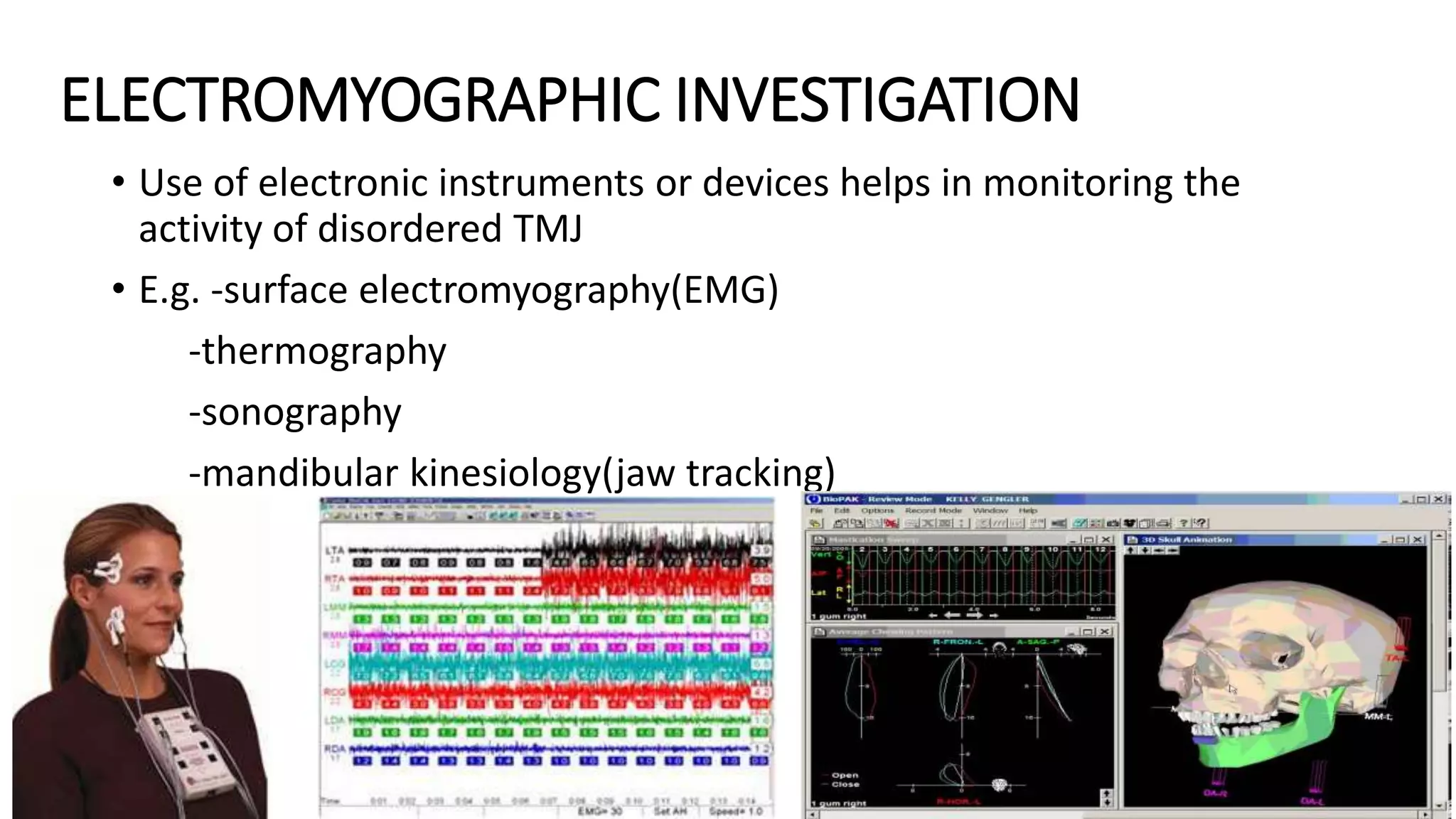
The second paragraph classifies TMDs as either intra-articular/intrinsic disorders involving the joint itself, or extra-articular/extrinsic disorders caused by factors outside the joint like muscle disorders, trauma