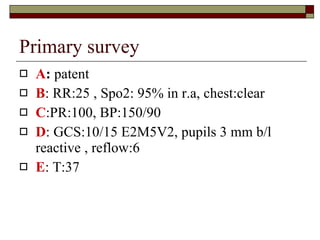
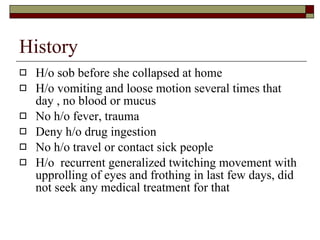
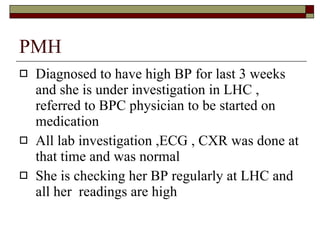
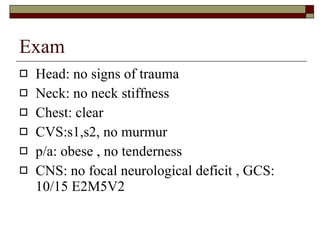
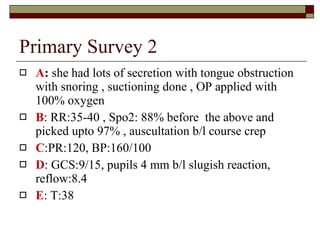
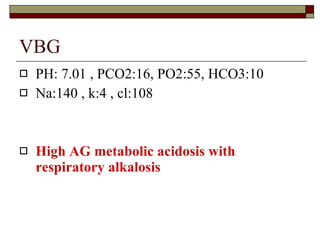
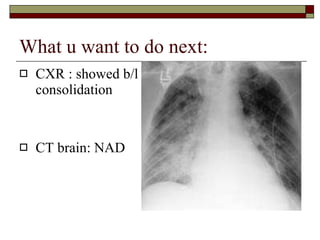
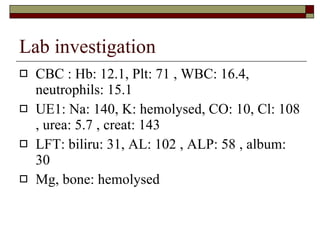
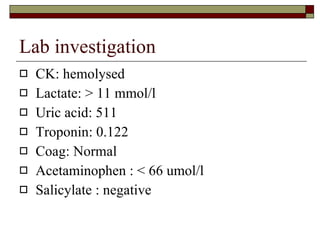
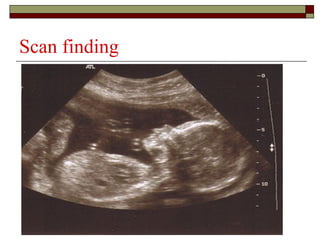
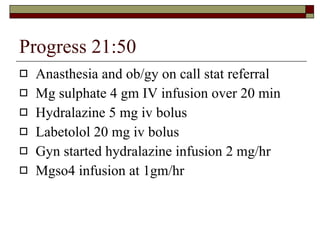
The document presents a case study of a 24-year-old female patient who was found unresponsive. Initial examination found the patient to have a Glasgow Coma Scale of 10/15, tachycardia, hypertension, and signs of respiratory distress. Laboratory tests revealed metabolic acidosis, elevated white blood cell count and creatinine, and rhabdomyolysis. Ultrasound showed signs of pregnancy. The patient was treated for pre-eclampsia with magnesium sulfate and antihypertensives, intubated, and underwent termination of pregnancy. She was admitted to the ICU and later discharged in good condition.