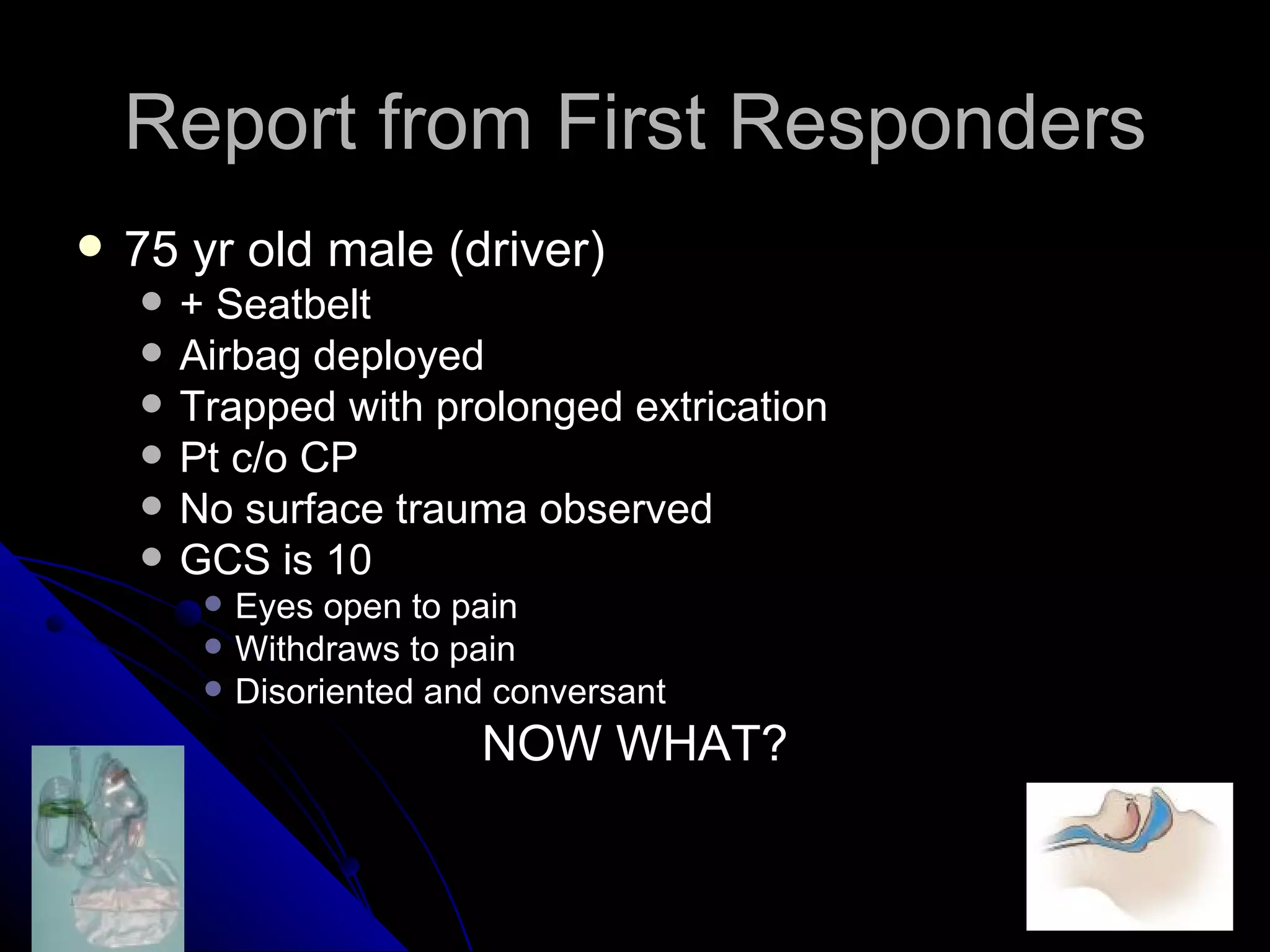
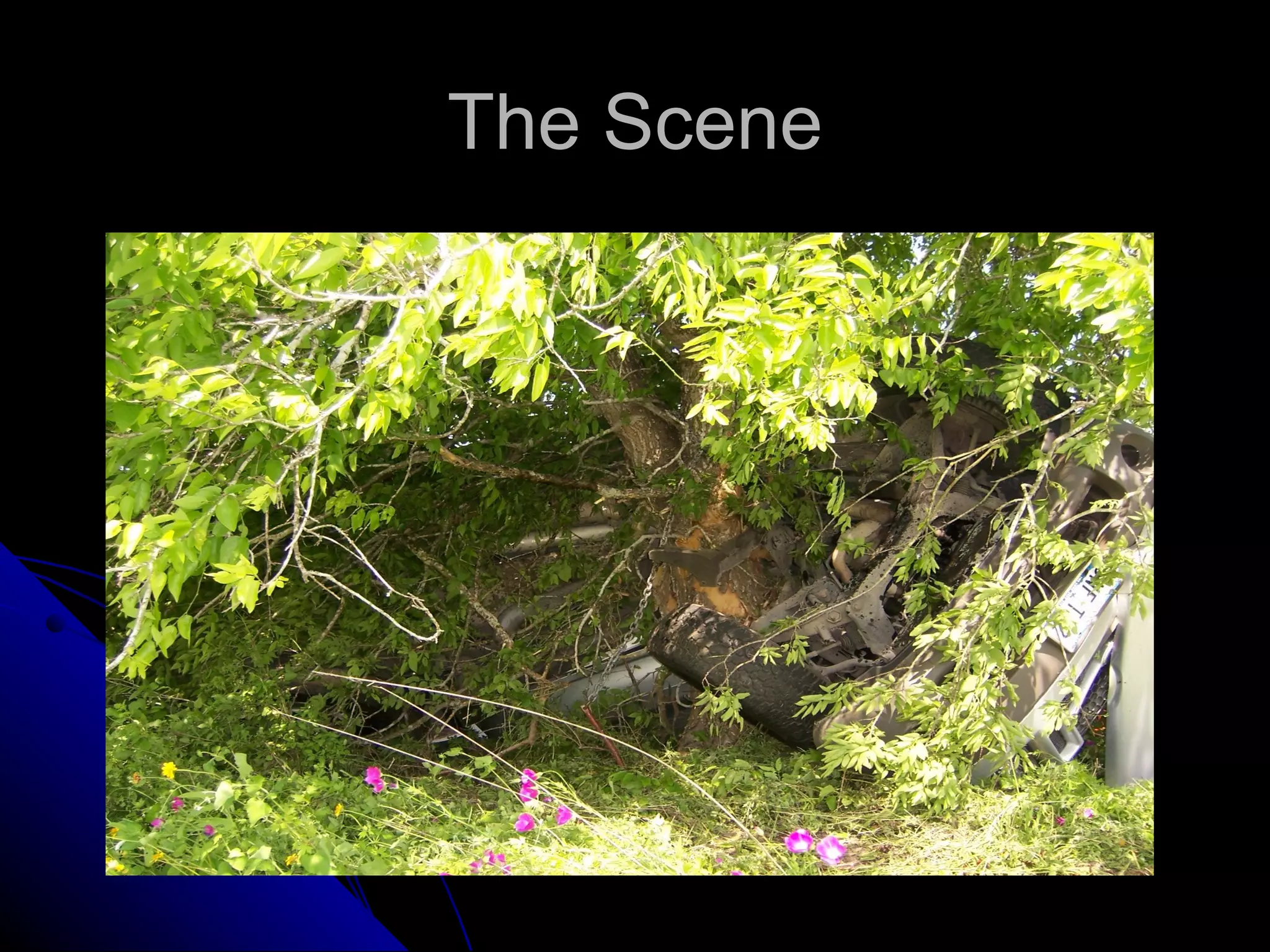
Let's review the imaging findings.
�Imaging Findings
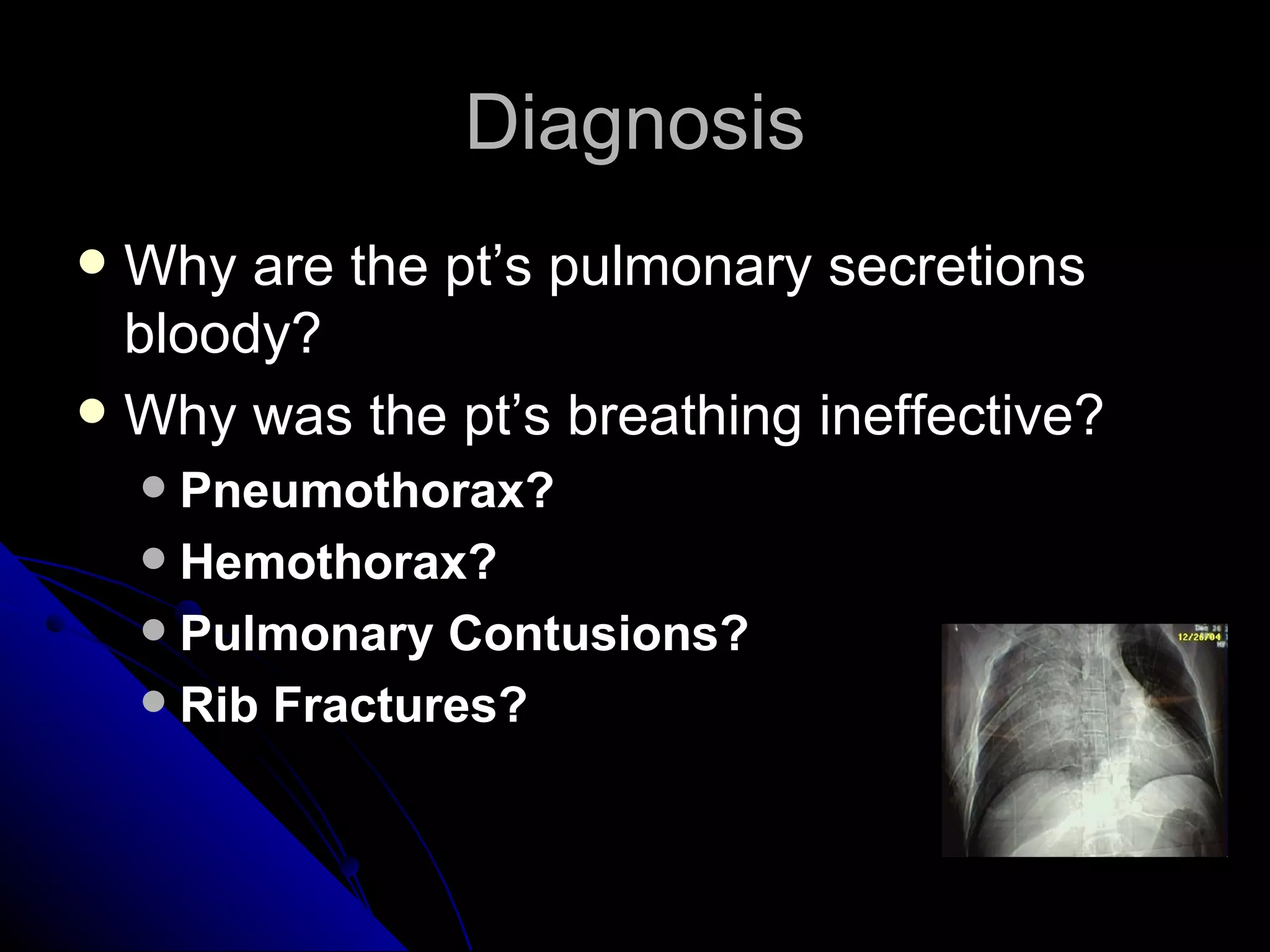
CXR:
- Bilateral pulmonary contusions
- Left sided hemopneumothorax
CT Chest:
- 5 left sided rib fractures
- Left hemopneumothorax
- Bilateral pulmonary contusions
- No aortic injury
- No cardiac tamponade
CT Head:
- No acute intracranial injury
CT C-Spine/Chest:
- No cervical spine injury
CT Abdomen/Pelvis:
- No intra-abdominal injury
- Stable pelvis
The imaging confirms pulmonary contusions and hemopneumothorax