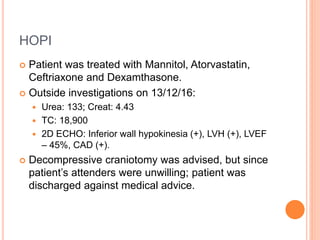
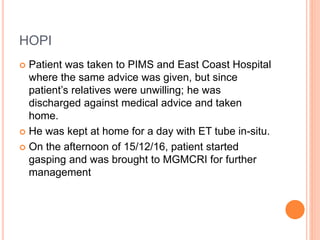
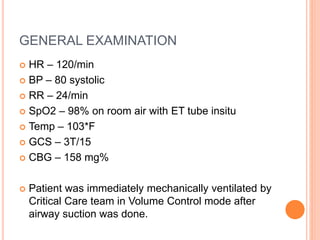
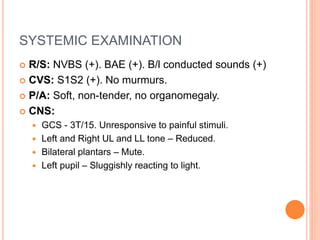
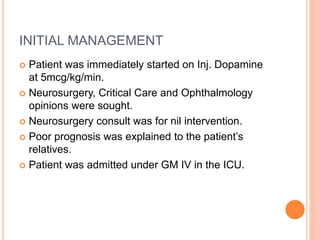
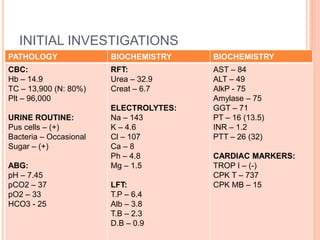
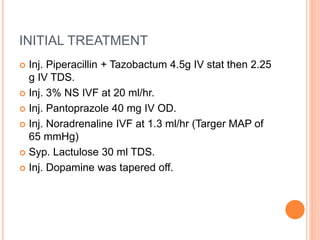
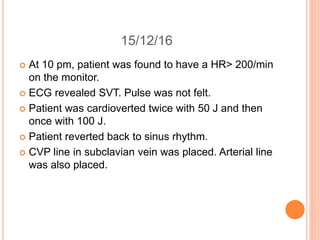
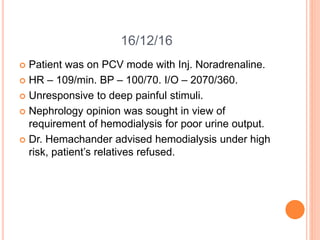
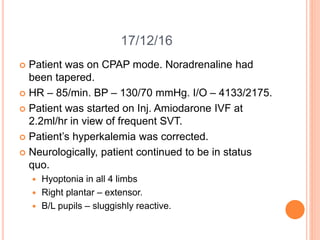
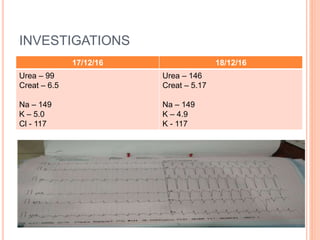
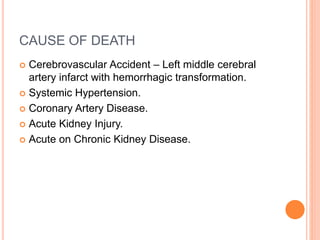
This document summarizes a death audit report for a 67-year-old male patient who passed away after being admitted for 3 days. The patient initially presented unconscious after suffering a stroke. He developed complications including heart arrhythmias, kidney injury, and deteriorating neurological function. Despite attempts at resuscitation, the patient went into asystole and could not be revived. The causes of death were determined to be a cerebrovascular accident exacerbated by underlying conditions of hypertension, coronary artery disease, and kidney injury.