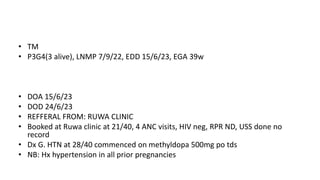
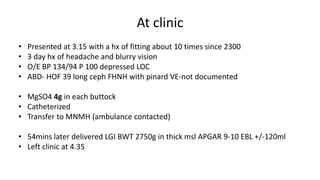
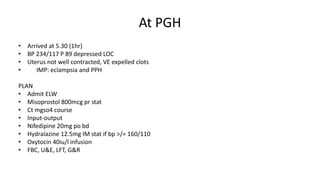
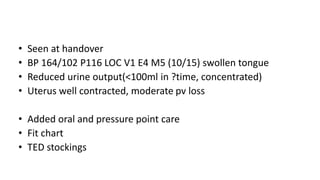
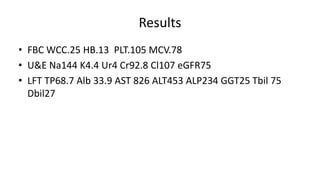
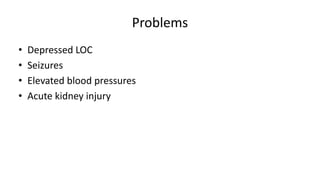
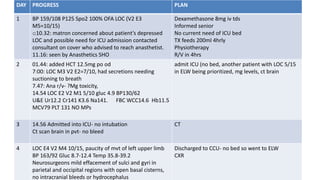
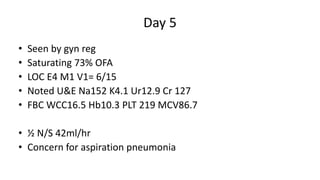
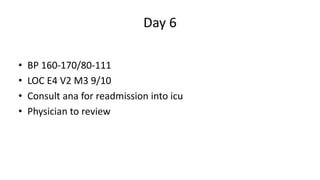
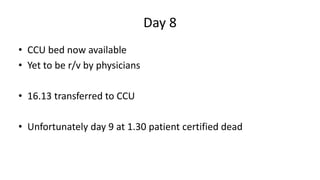
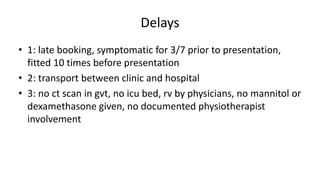
The document details a maternal mortality case, highlighting the patient's history of hypertension and eclampsia, alongside her presenting symptoms which included seizures and elevated blood pressure. Despite treatment efforts, including medication and monitoring, the patient ultimately passed away, with contributing factors identified as late booking, transport delays, and lack of resources. Recommendations include improving patient education, standardizing care practices, and enhancing hospital resource availability.