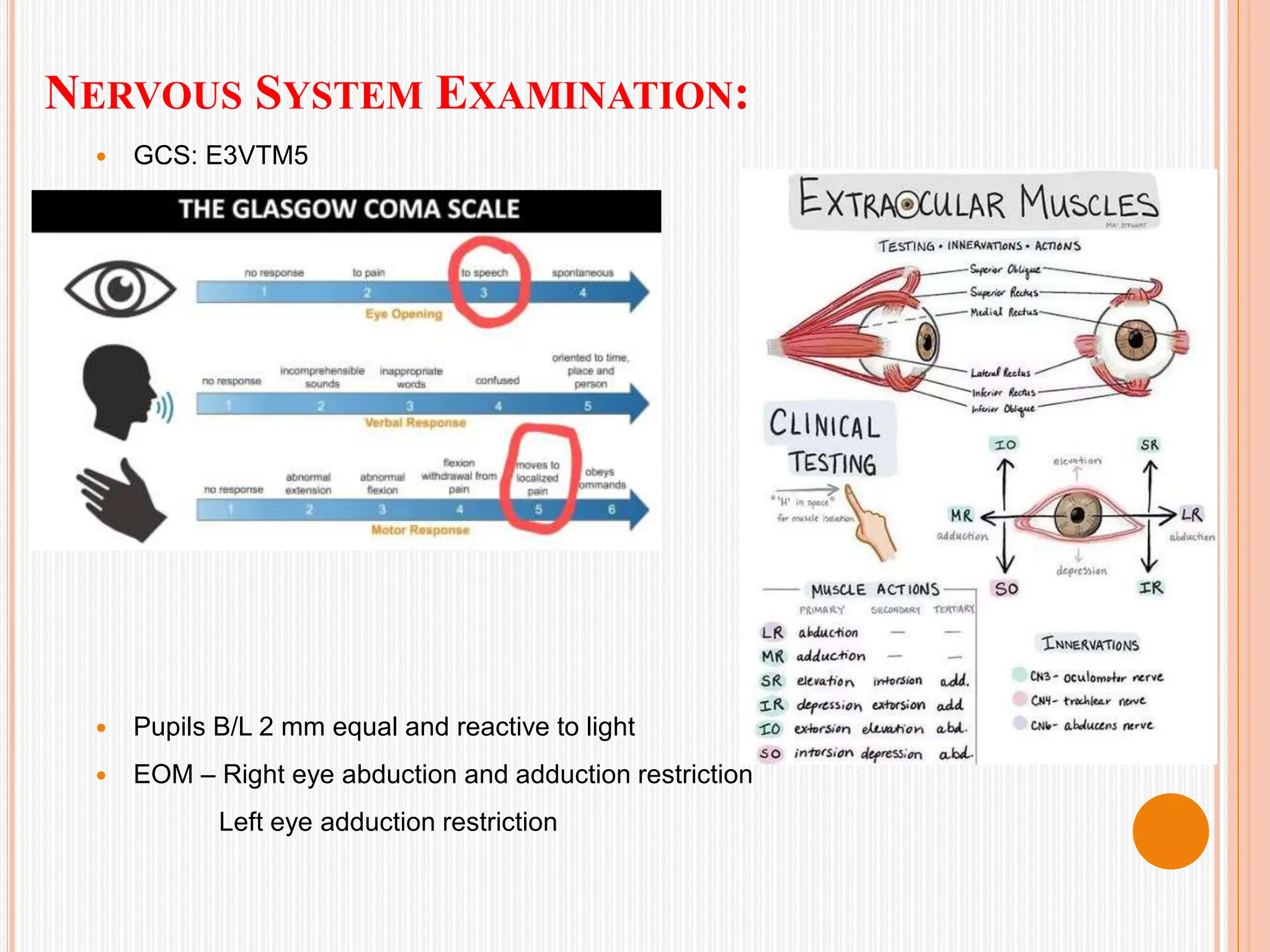
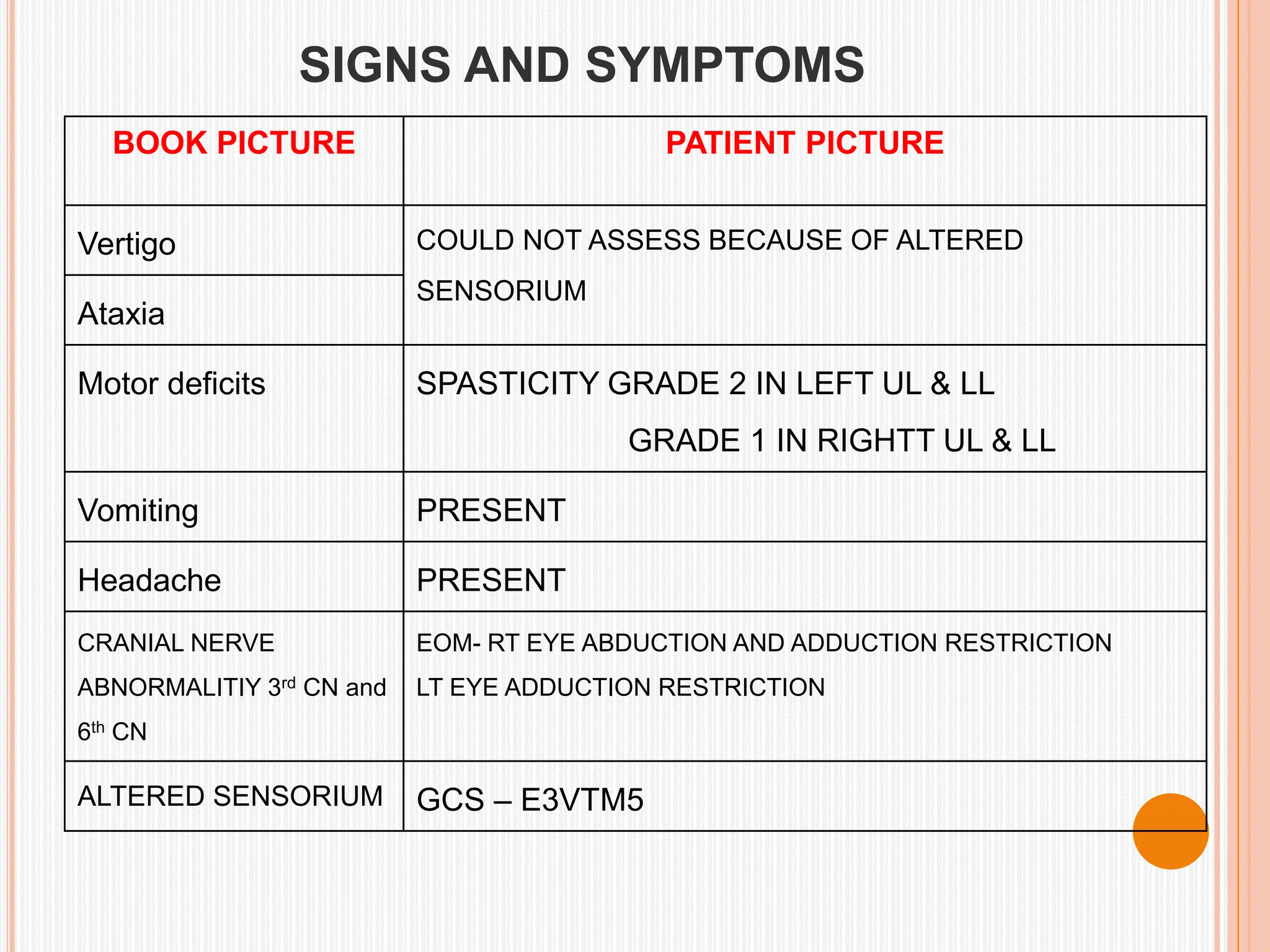
A 28-year-old female presented with neck pain, vomiting, and unconsciousness after being diagnosed with a posterior circulation stroke due to a dissecting aneurysm and antiphospholipid syndrome. She received extensive medical treatment, including intubation, mechanical ventilation, and rehabilitation, ultimately leading to her discharge on 17.04.2024 in stable condition. The case highlights the complexities of acute stroke management and the interdisciplinary approach required for recovery.