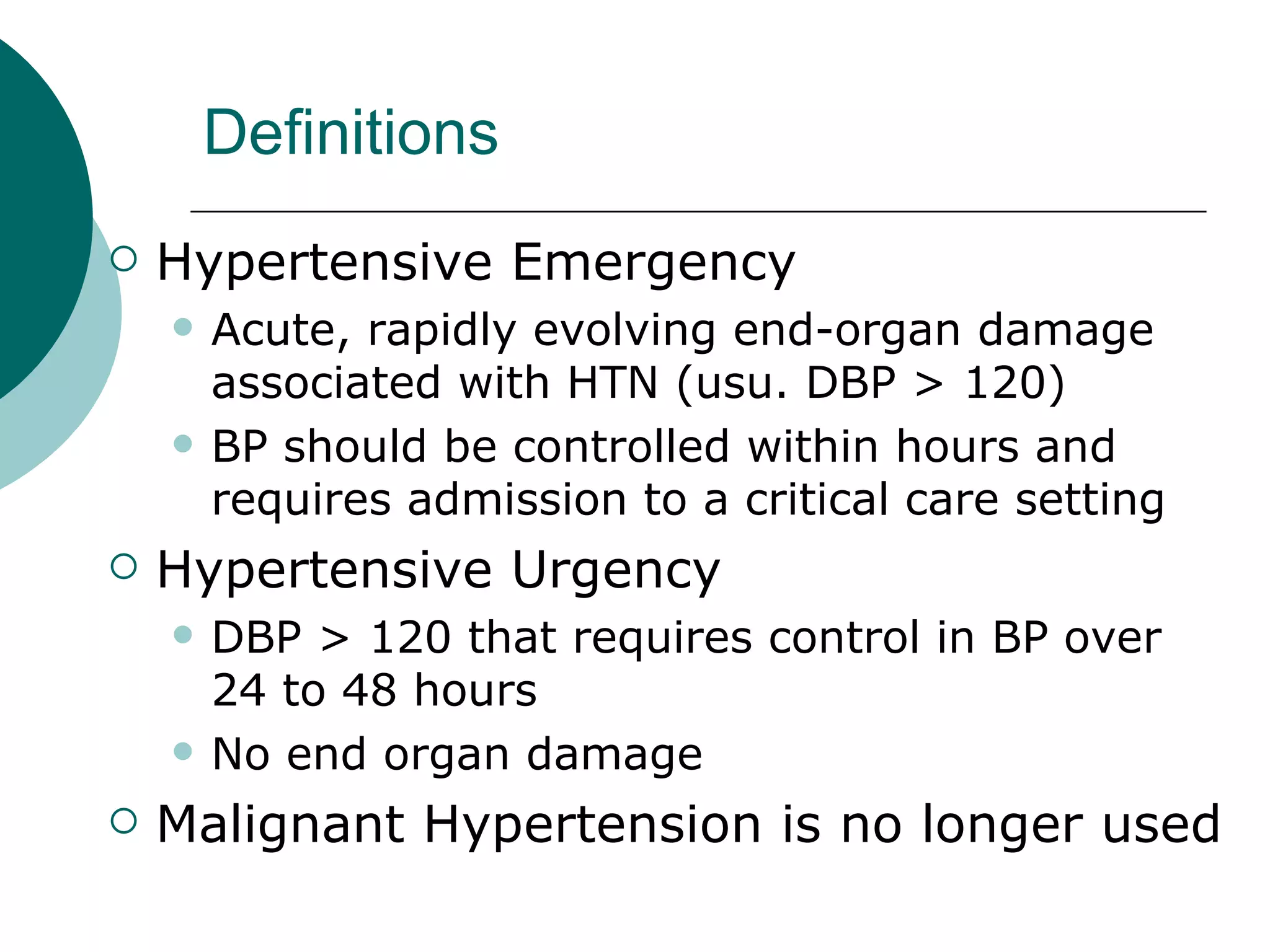
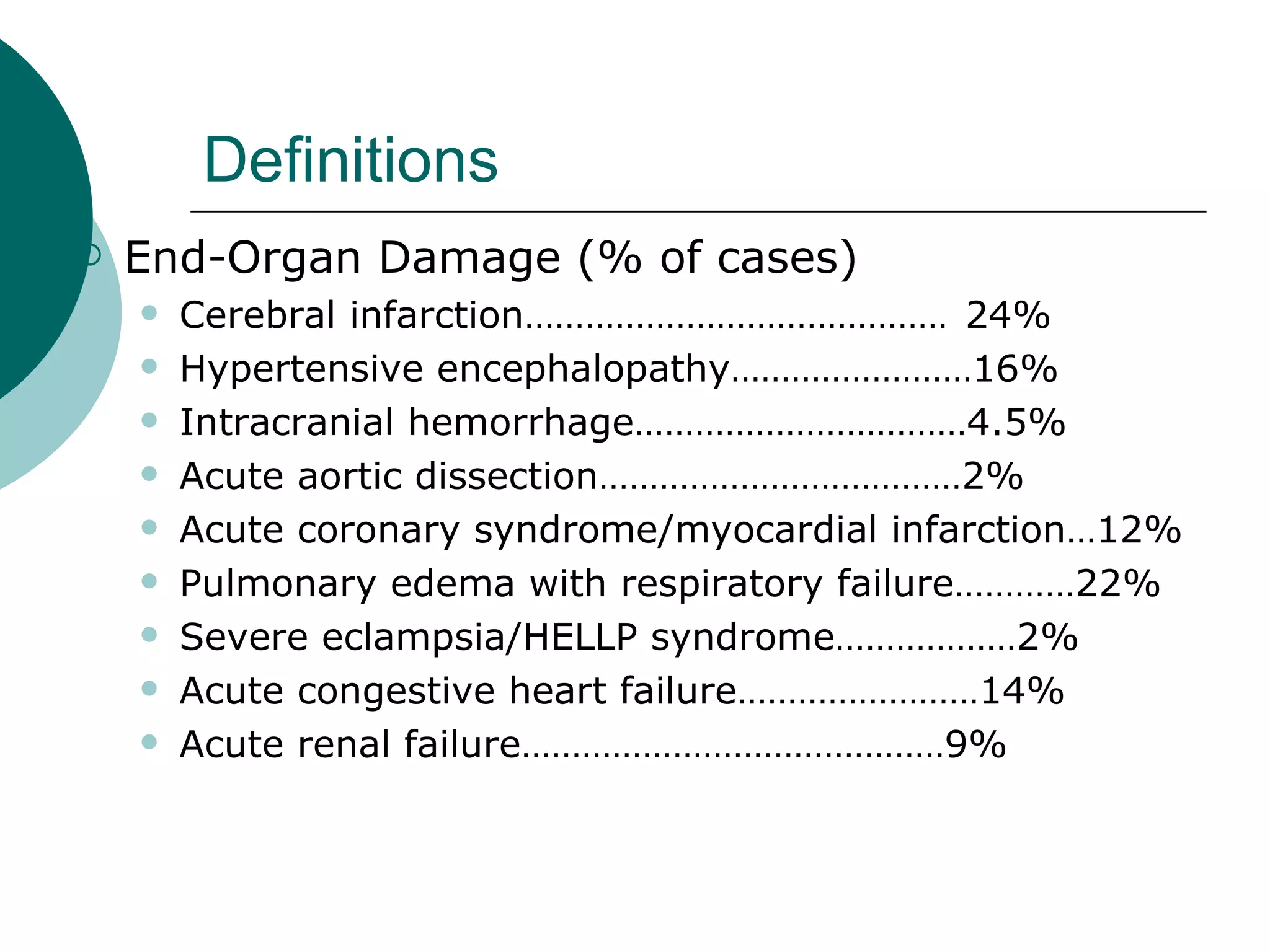
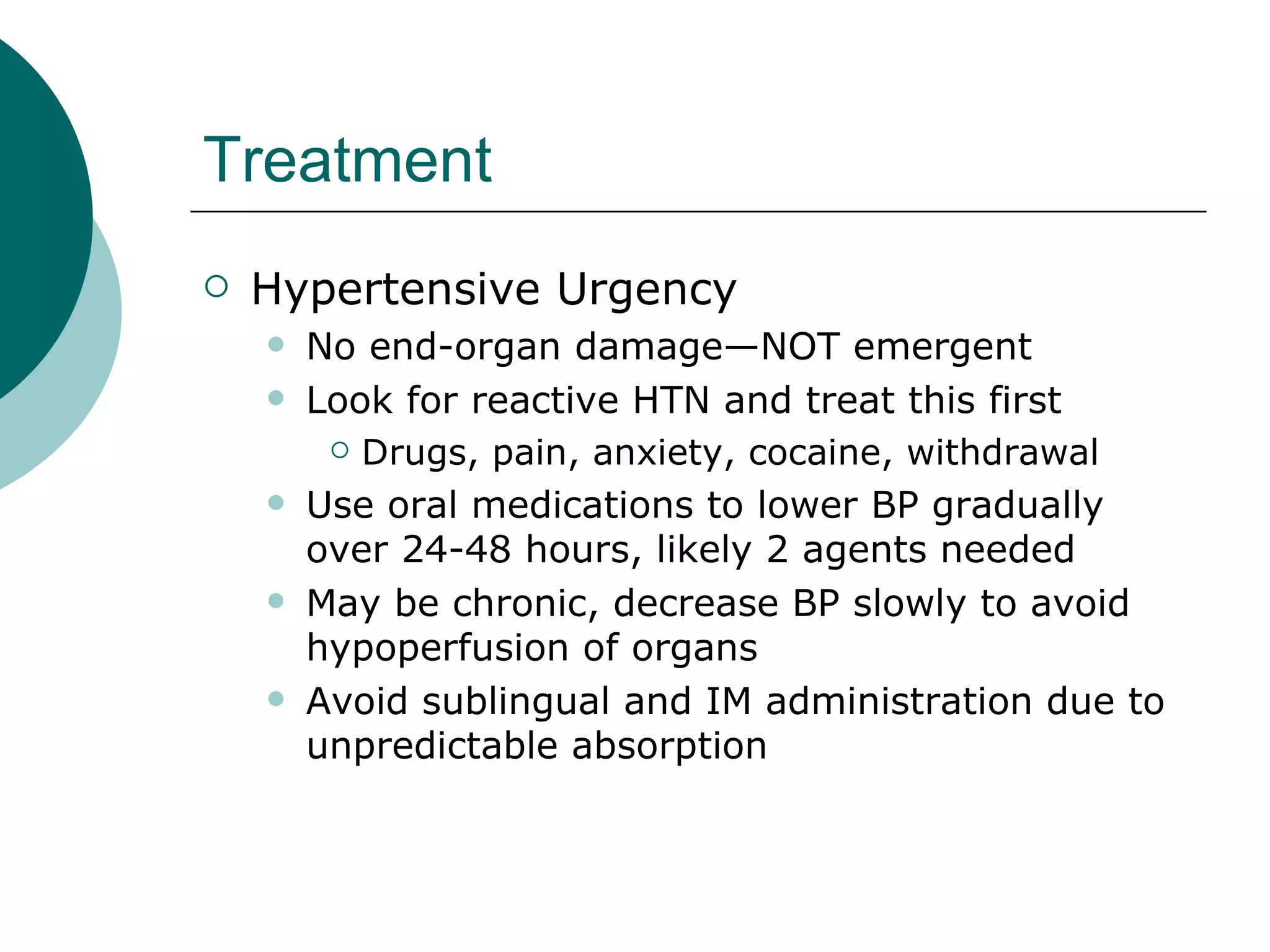
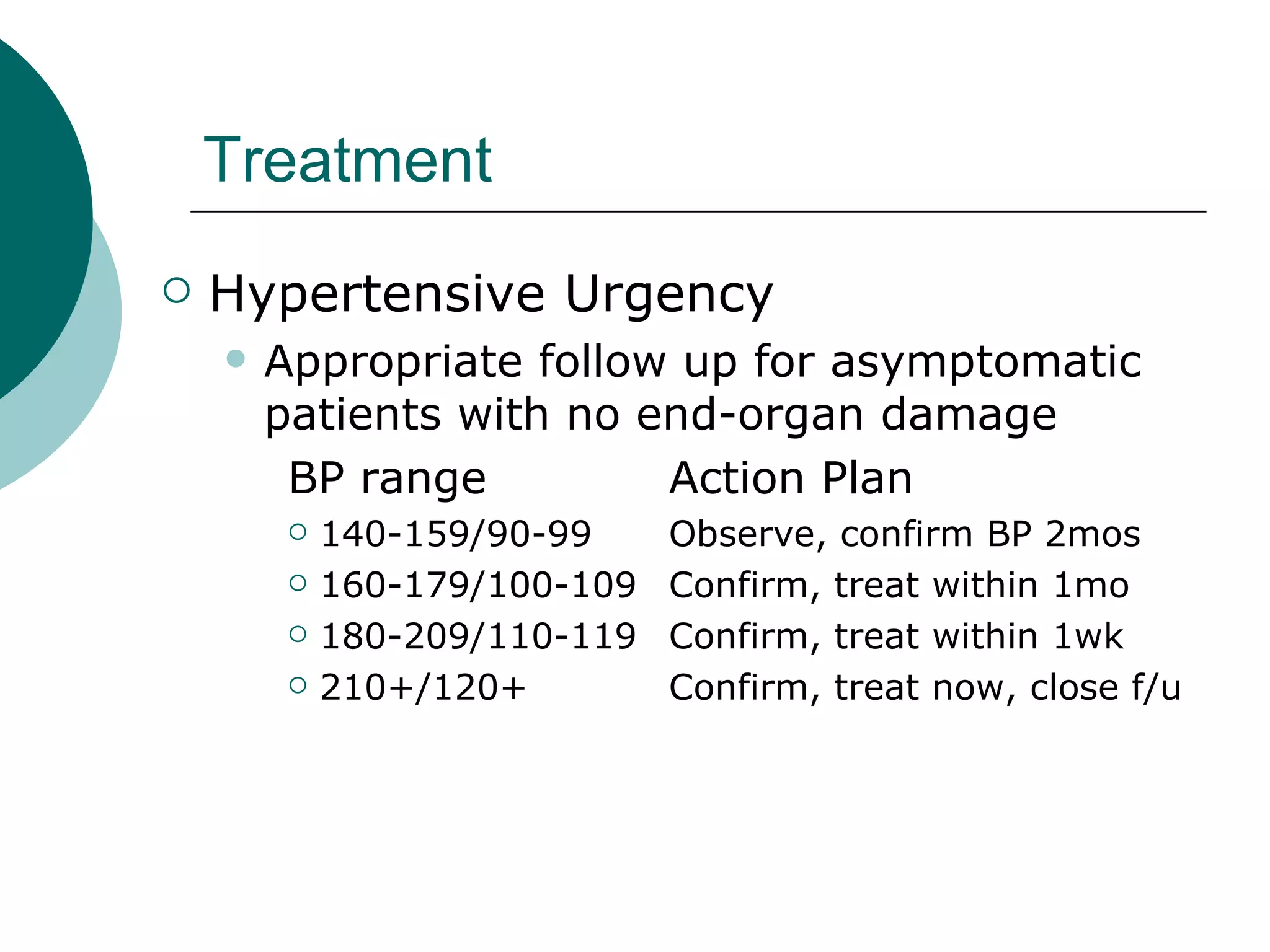
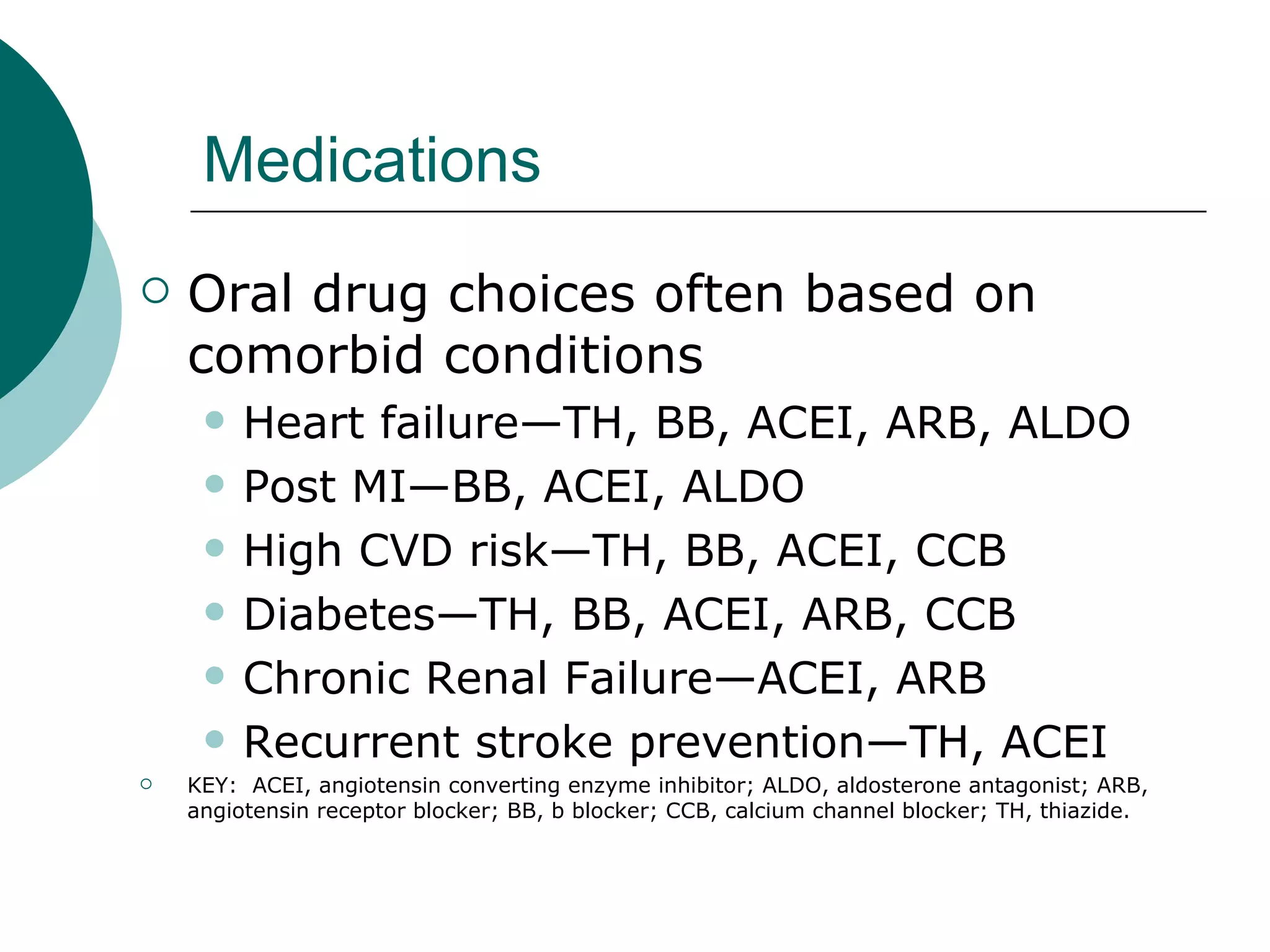
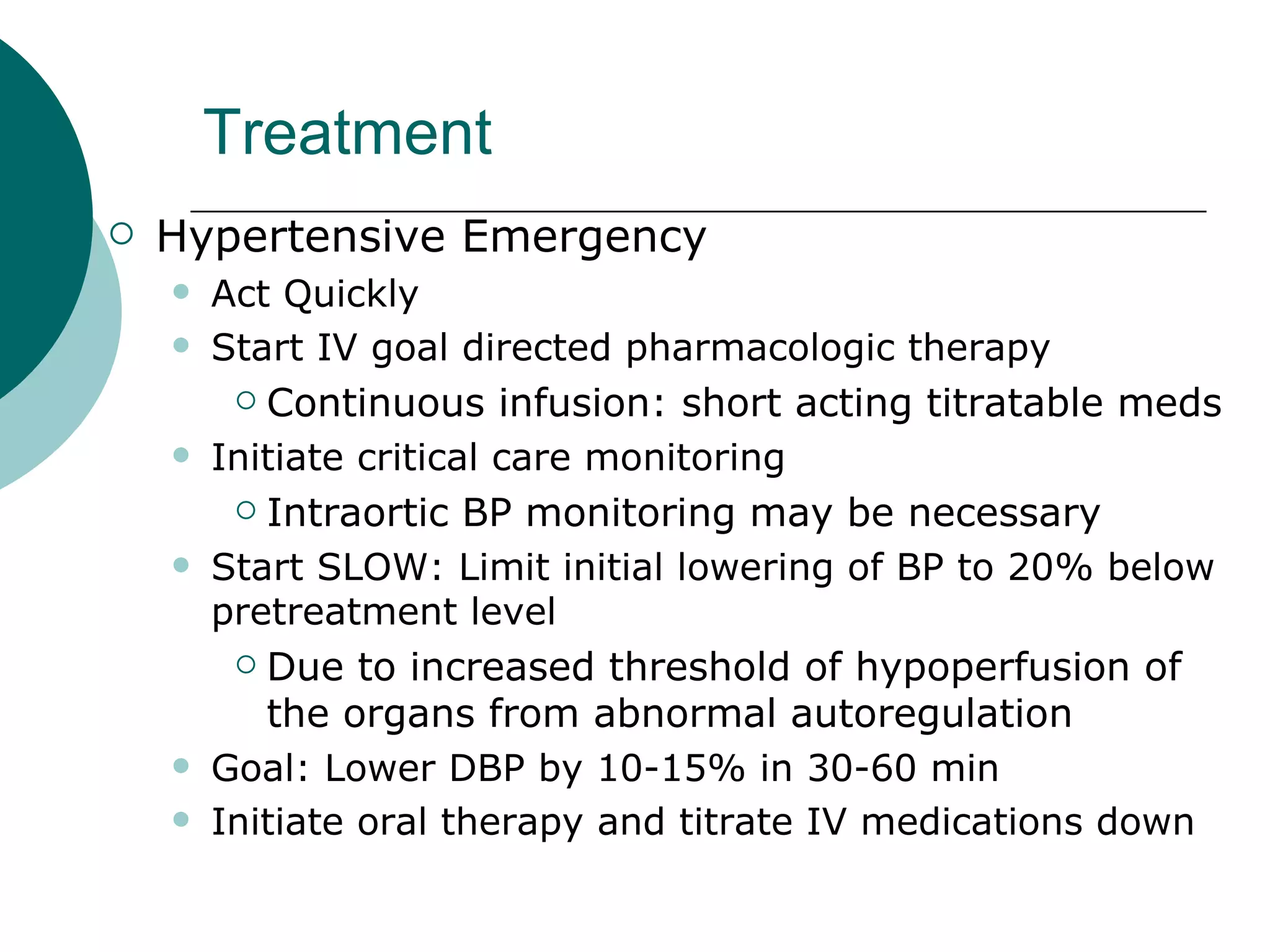
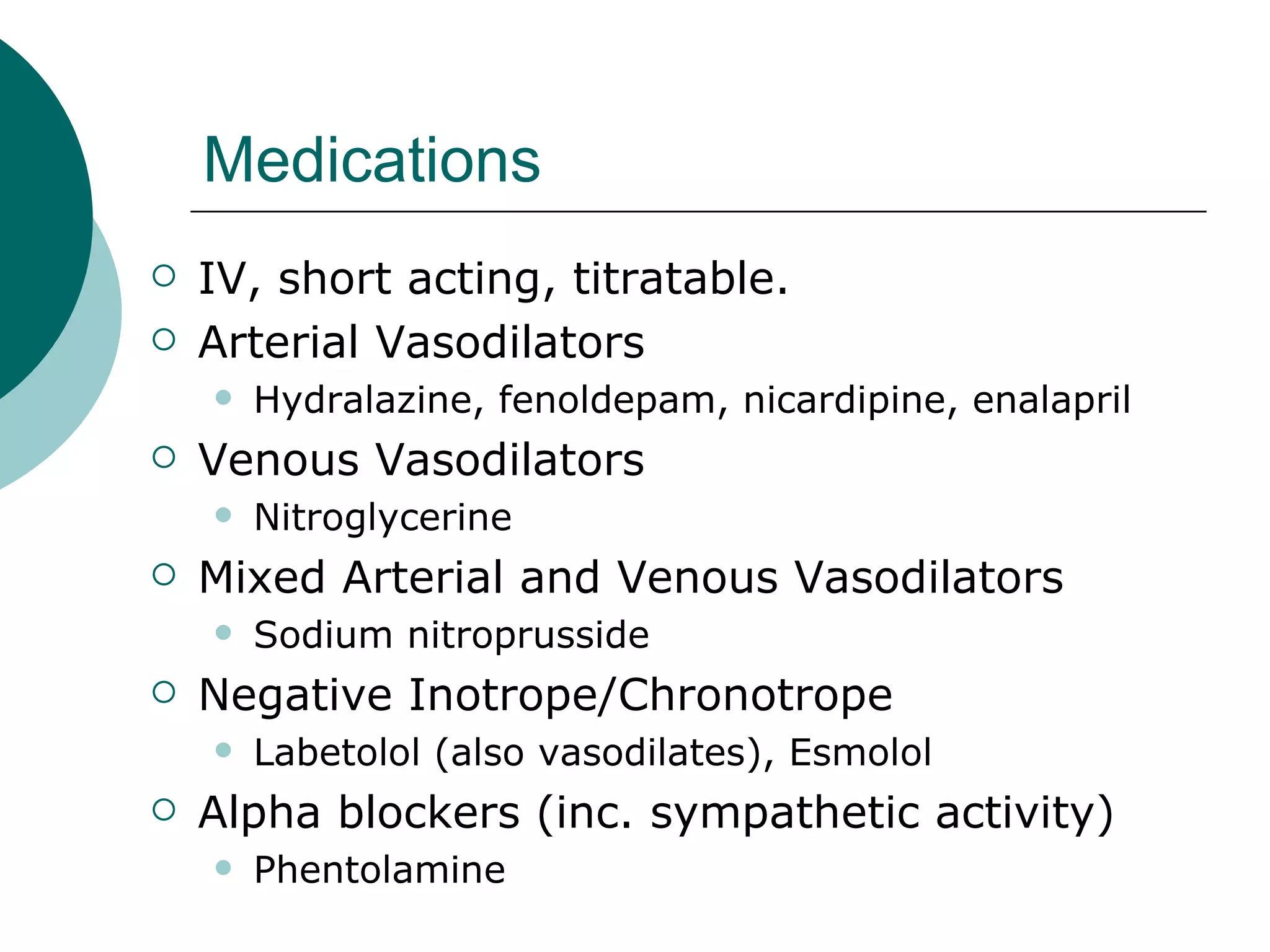
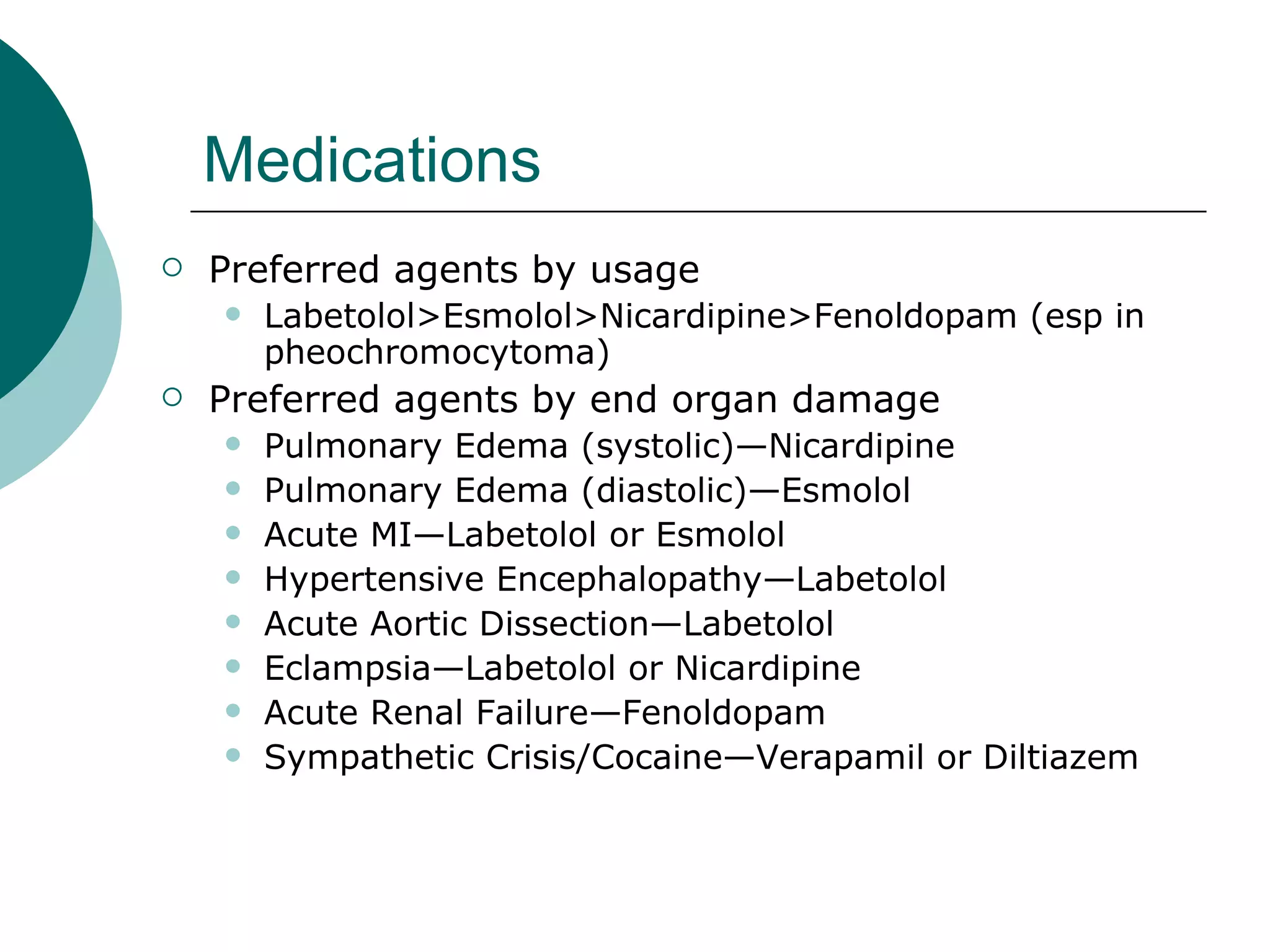
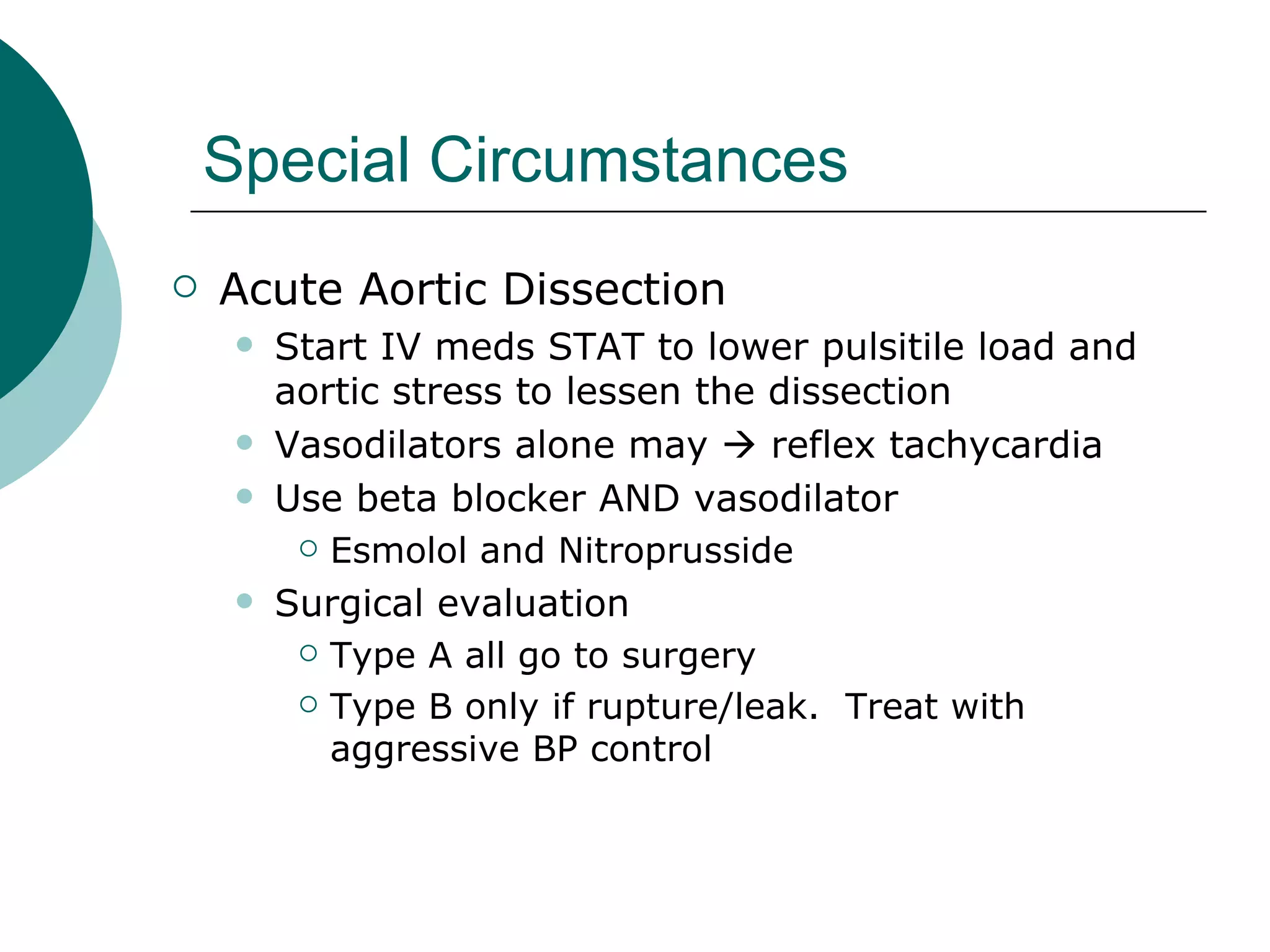
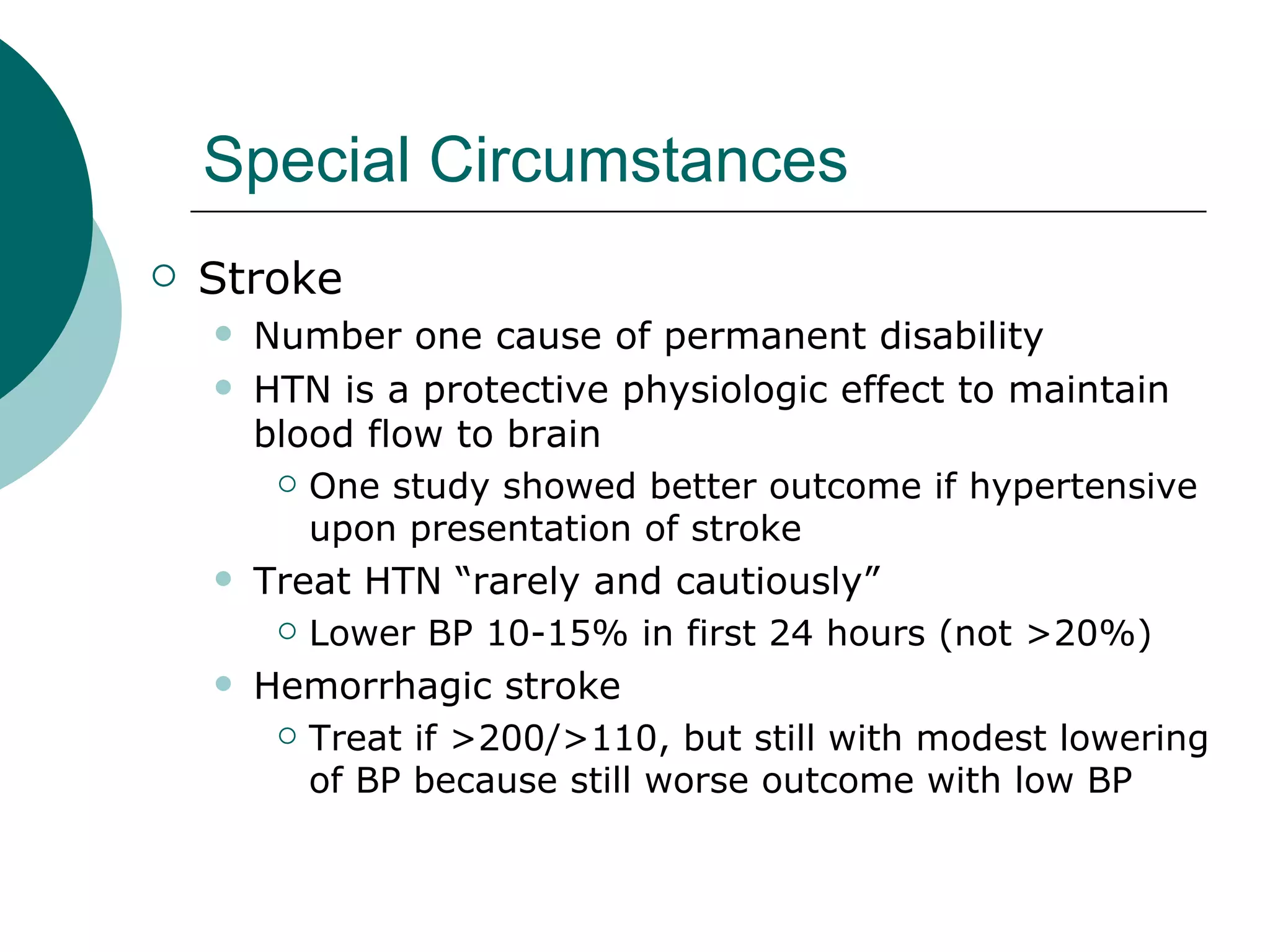
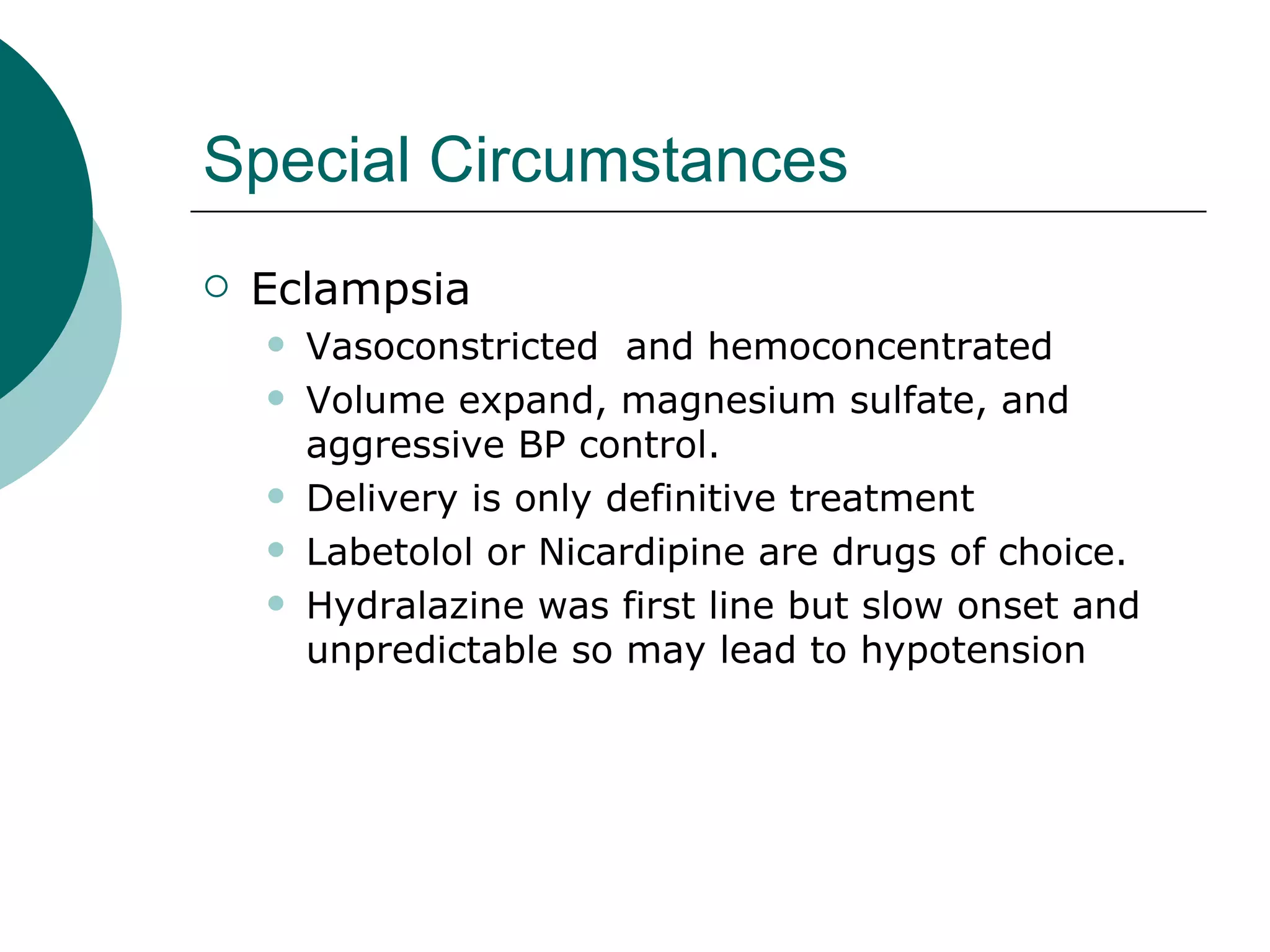
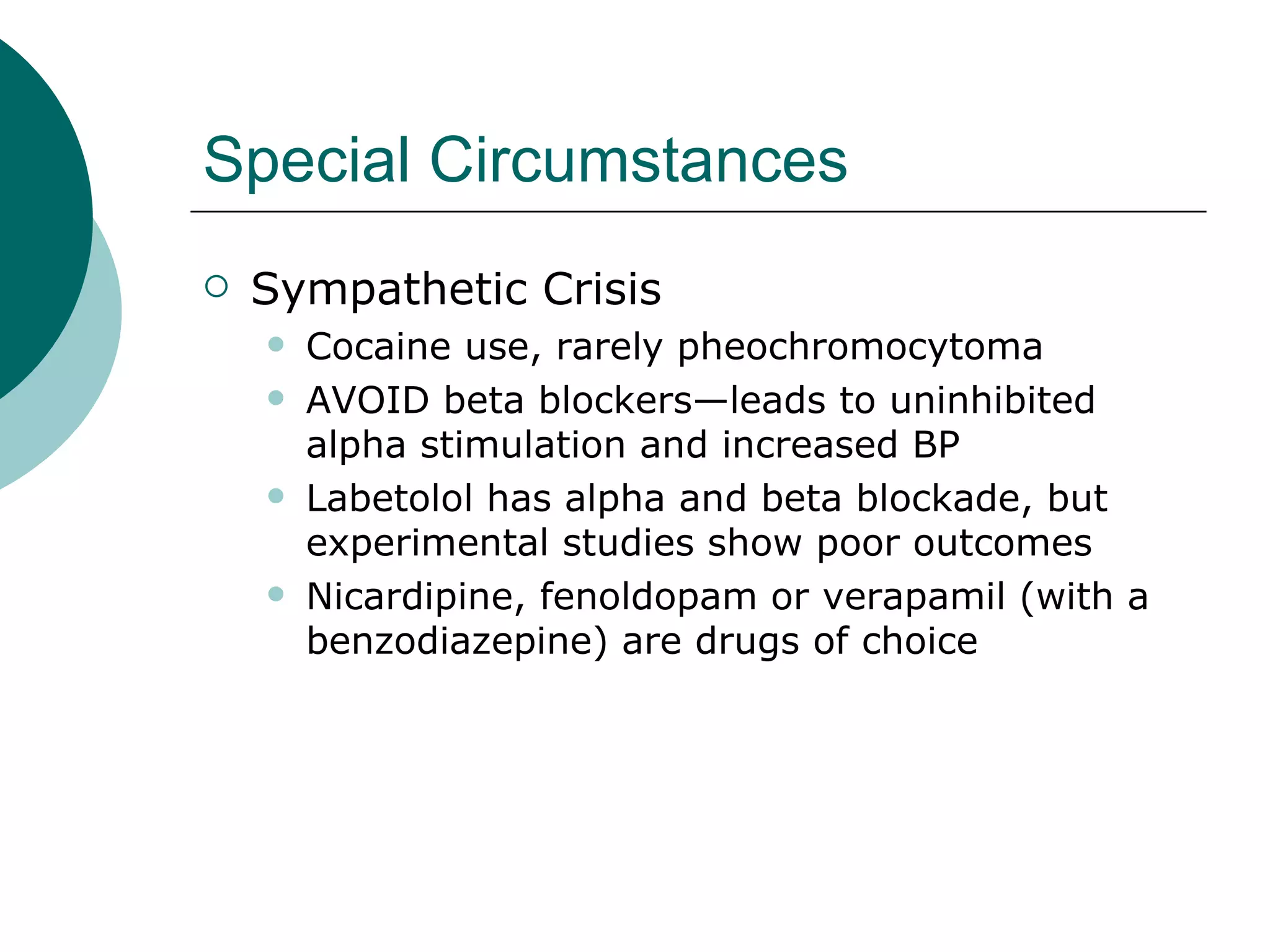
This document discusses hypertensive emergencies. It defines hypertensive emergency as acute end-organ damage from severely high blood pressure that requires rapid control. Over 500,000 Americans experience this each year. Treatment involves quickly starting intravenous drugs to lower blood pressure 20% within 60 minutes to prevent further damage, while oral medications are initiated. Conditions like stroke, aortic dissection and eclampsia may require specific approaches. Rapid diagnosis and management of hypertensive emergencies is critical to reducing mortality rates that can be as high as 90%.