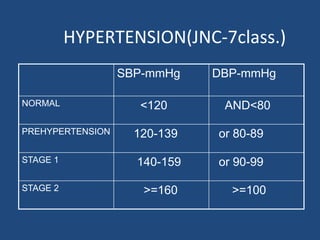
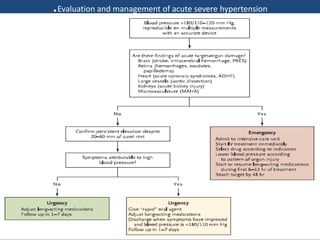
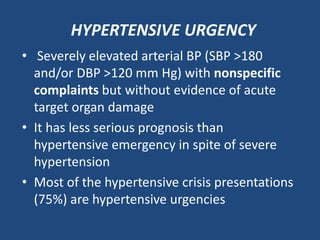
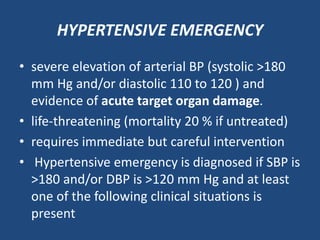
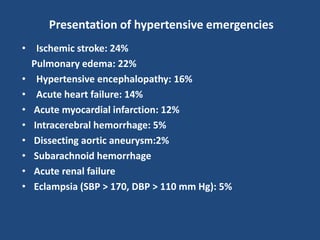
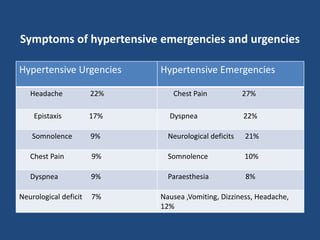
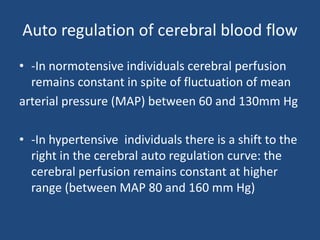
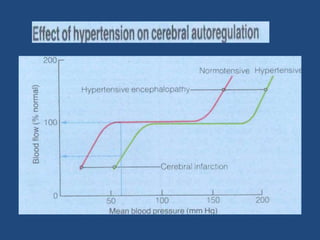
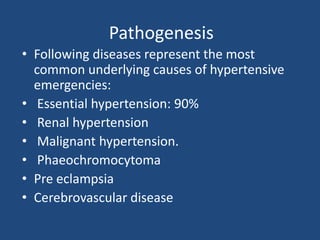
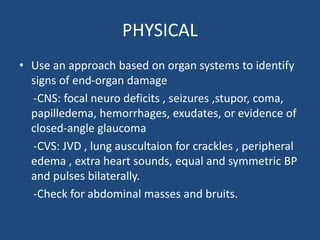
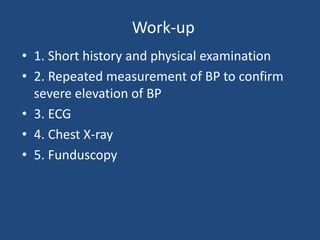
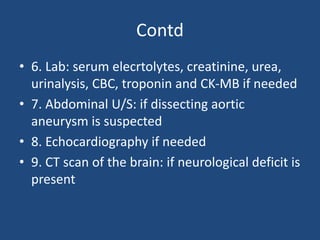
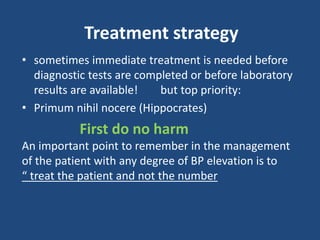
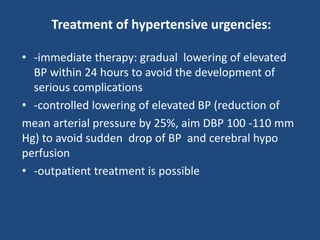
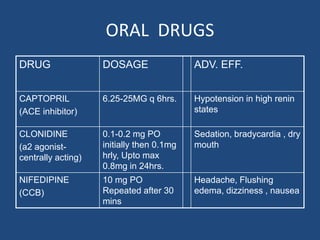
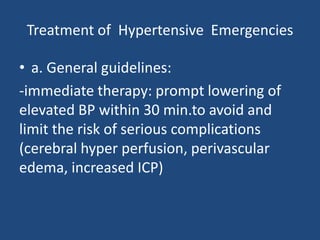
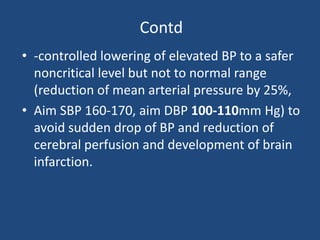
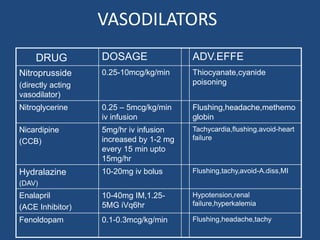
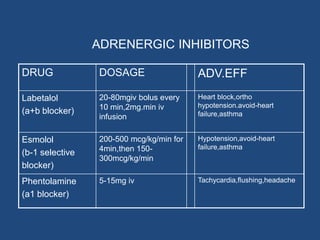
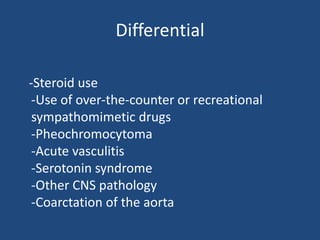
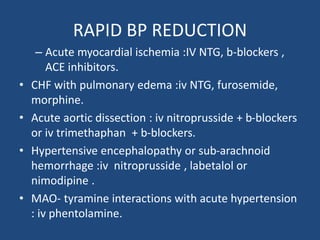
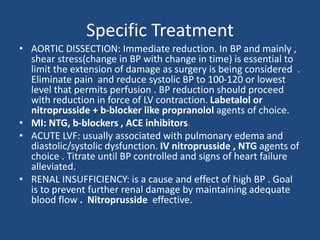
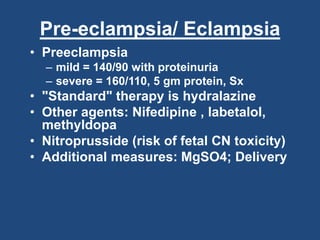
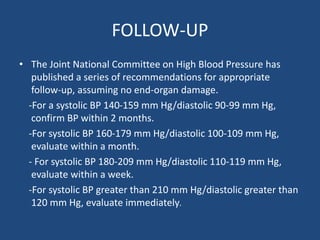
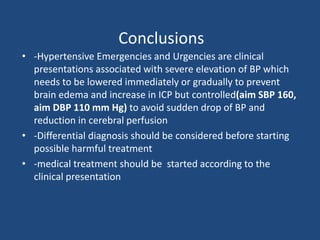
Hypertension is defined as blood pressure above 140/90 mmHg or use of antihypertensive medication. Hypertensive emergencies involve severe elevation of blood pressure and evidence of acute target organ damage, requiring immediate but careful intervention to lower blood pressure within 30 minutes. Hypertensive urgencies involve severely elevated blood pressure without organ damage, allowing more gradual blood pressure reduction over 24 hours as an outpatient. Treatment depends on the clinical presentation and may include vasodilators like nitroprusside or adrenergic inhibitors like labetalol to carefully lower blood pressure while avoiding complications of too rapid a decrease.