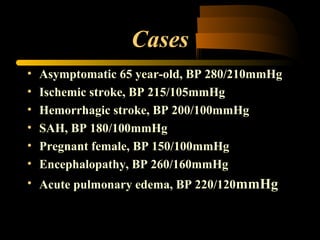
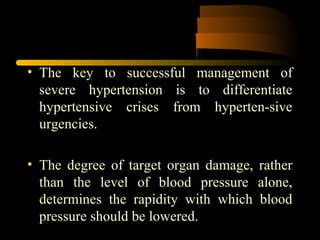
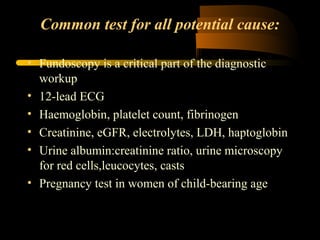
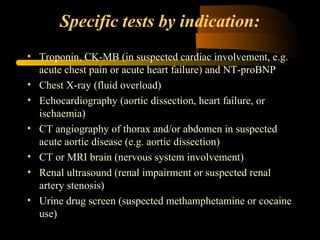
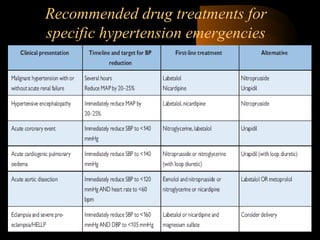
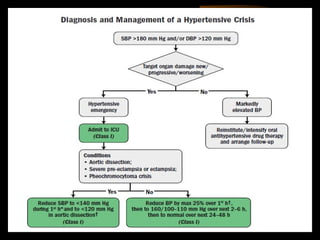
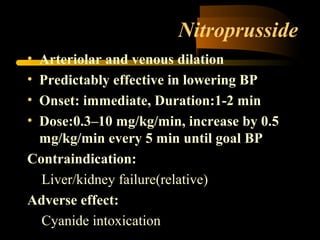
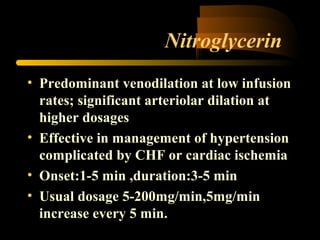
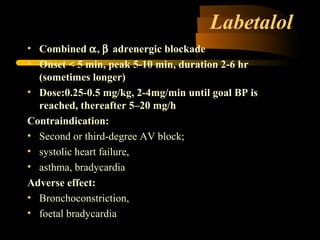
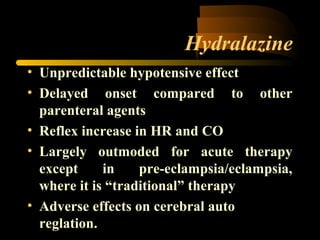
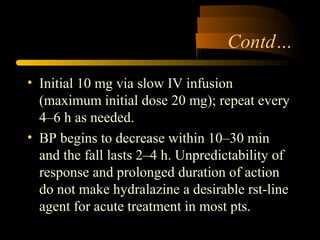
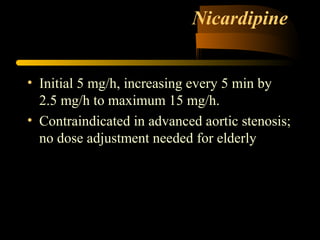
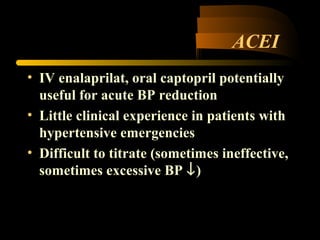
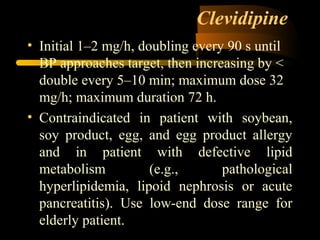
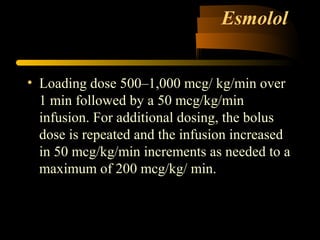
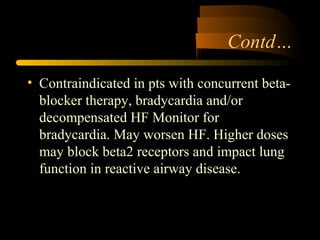
This document summarizes a clinical meeting on hypertensive emergencies. It defines hypertensive emergencies as severe hypertension associated with acute organ damage that requires immediate but careful intervention. It outlines objectives to distinguish presentations requiring therapy, describe appropriate therapies and risks, and discuss antihypertensive drugs. It then provides cases and defines malignant hypertension and other presentations. It discusses evaluating organ damage, recommended drug treatments like nitroprusside, labetalol, and nicardipine, and emphasizes lowering blood pressure no more than 25% within 2 hours. The document concludes that patients have improved survival but remain at high risk, requiring frequent follow-up after discharge.