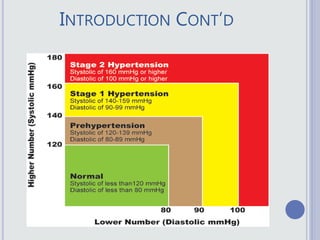
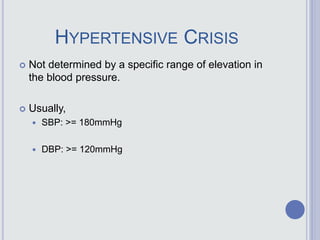
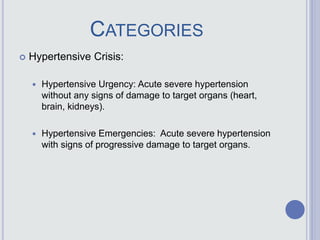
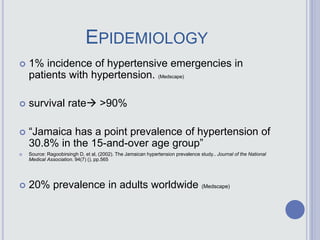
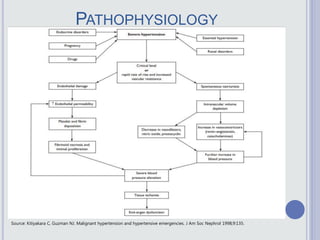
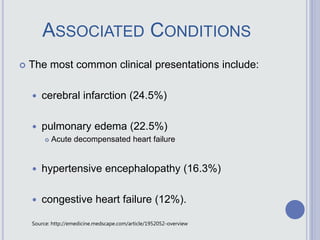
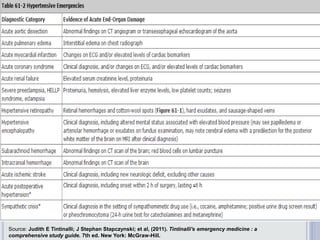
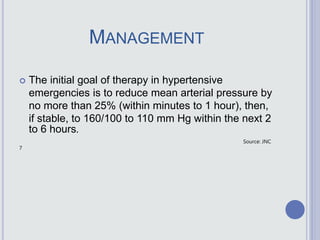
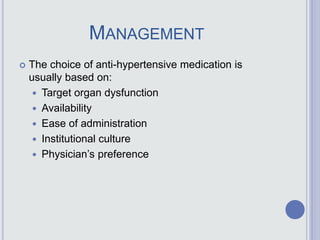
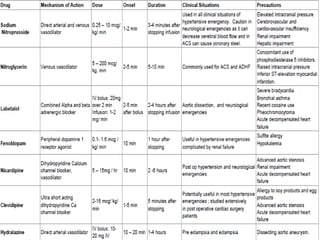
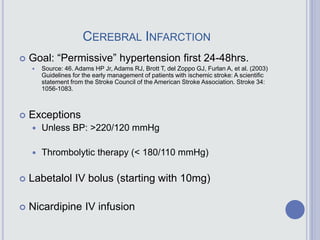
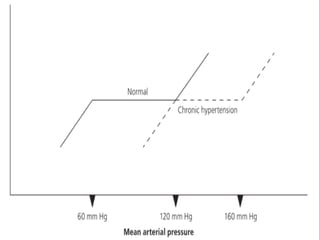
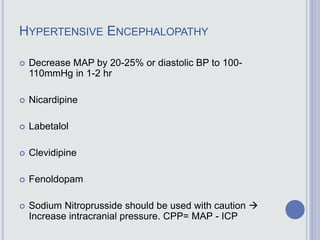
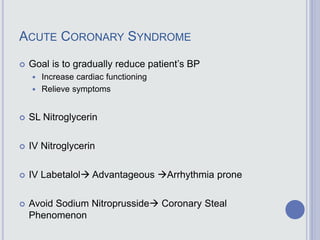
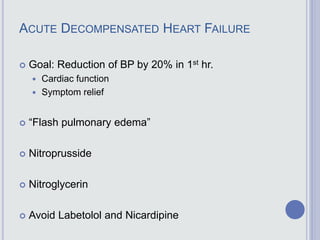
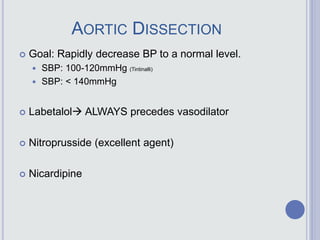
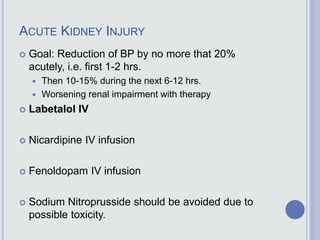
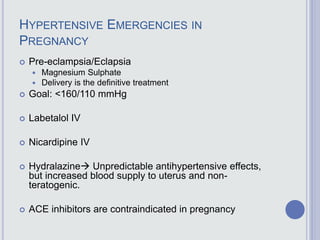
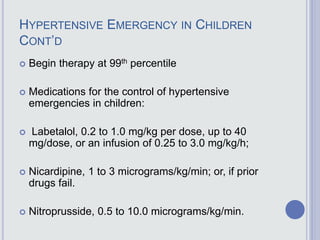
This document defines hypertensive emergencies and discusses their management. It begins by classifying hypertension and defining hypertensive crises. Hypertensive emergencies are acute severe hypertension with signs of target organ damage, while hypertensive urgencies have severe hypertension without organ damage. The document then covers the epidemiology, etiology, pathophysiology, presentation, investigations, and management of hypertensive emergencies. It discusses treating different organ-specific emergencies like stroke, heart failure, and kidney injury. The management involves rapid blood pressure reduction while monitoring for complications. Various intravenous medications are outlined to treat specific emergencies. Careful titration is needed due to the risk of overtreatment.


![REFERENCES
Mahadevan S.V. & Garmel G. M., (2005). An Introduction to Clinical
Emergency Medicine Guide for Practitioners in the Emergency
Department. 1st ed. United States of America: Cambridge University
Press.
Bakris G. L. (2014). Hypertensive Emergencies. [ONLINE] Available
at:
http://www.merckmanuals.com/professional/cardiovascular_disorders
/hypertension/hypertensive_emergencies.html. [Last Accessed 28
December 14].
Madhur M.S., et al. (2014). Hypertension. [ONLINE] Available at:
http://emedicine.medscape.com/article/241381-
overview#aw2aab6b2b2. [Last Accessed 28/12/14].
Judith E Tintinalli; J Stephan Stapczynski; et al, (2011). Tintinalli's
emergency medicine : a comprehensive study guide. 7th ed. New
York: McGraw-Hill.](https://image.slidesharecdn.com/hypertensiveemergencies-160418043048/85/Hypertensive-emergencies-43-320.jpg)
![REFERENCES
Vaidya C.K.& Oullette J.R. (2007). Hypertensive Urgency and
Emergency. [ONLINE] Available at: http://turner-
white.com/memberfile.php?PubCode=hp_mar07_hypertensive.p
df. [Last Accessed 21/1/15].
Shusterman NH, Elliott WJ, White WB (1993)
Fenoldopam, but not nitroprusside, improves renal
function in severely hypertensive patients with impaired
renal function. Am J Med 95: 161-168.
Elliott WJ, Weber RR, Nelson KS, Oliner CM, Fumo MT,
et al. (1990) Renal and hemodynamic effects of
intravenous fenoldopam versus nitroprusside in severe
hypertension. Circulation 81: 970-977.
Hopkins C., et al. (2013). Hypertensive Emergencies. [ONLINE] Available
at: http://emedicine.medscape.com/article/1952052-overview. [Last
Accessed 23/1/15].
Mallidi J, Penumetsa S, Lotfi A (2013) Management of
Hypertensive Emergencies. J Hypertens 2: 117](https://image.slidesharecdn.com/hypertensiveemergencies-160418043048/85/Hypertensive-emergencies-44-320.jpg)
