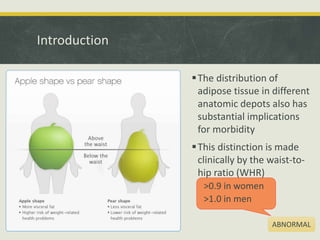
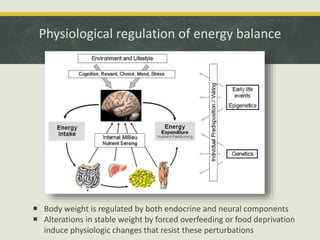
The document discusses obesity, defining it as an excess of adipose tissue and highlighting its physiological origins related to energy storage and survival. It emphasizes the health complications associated with obesity, including cardiovascular disease and diabetes, as well as the prevalence and measurement methods like BMI. Various treatments for obesity are outlined, including dietary changes, exercise, pharmacotherapy, and surgical options, all aimed at weight reduction and improving health outcomes.