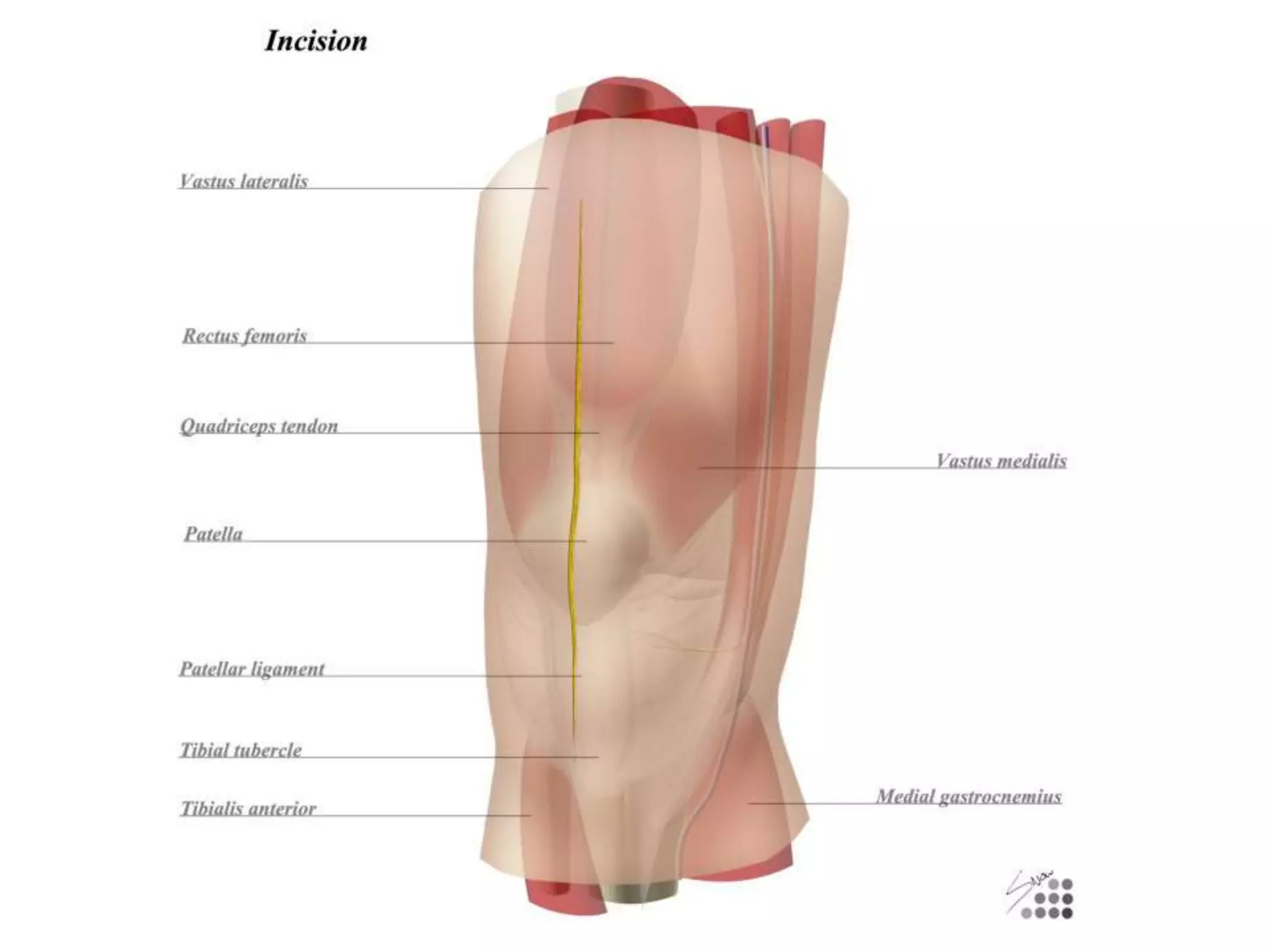
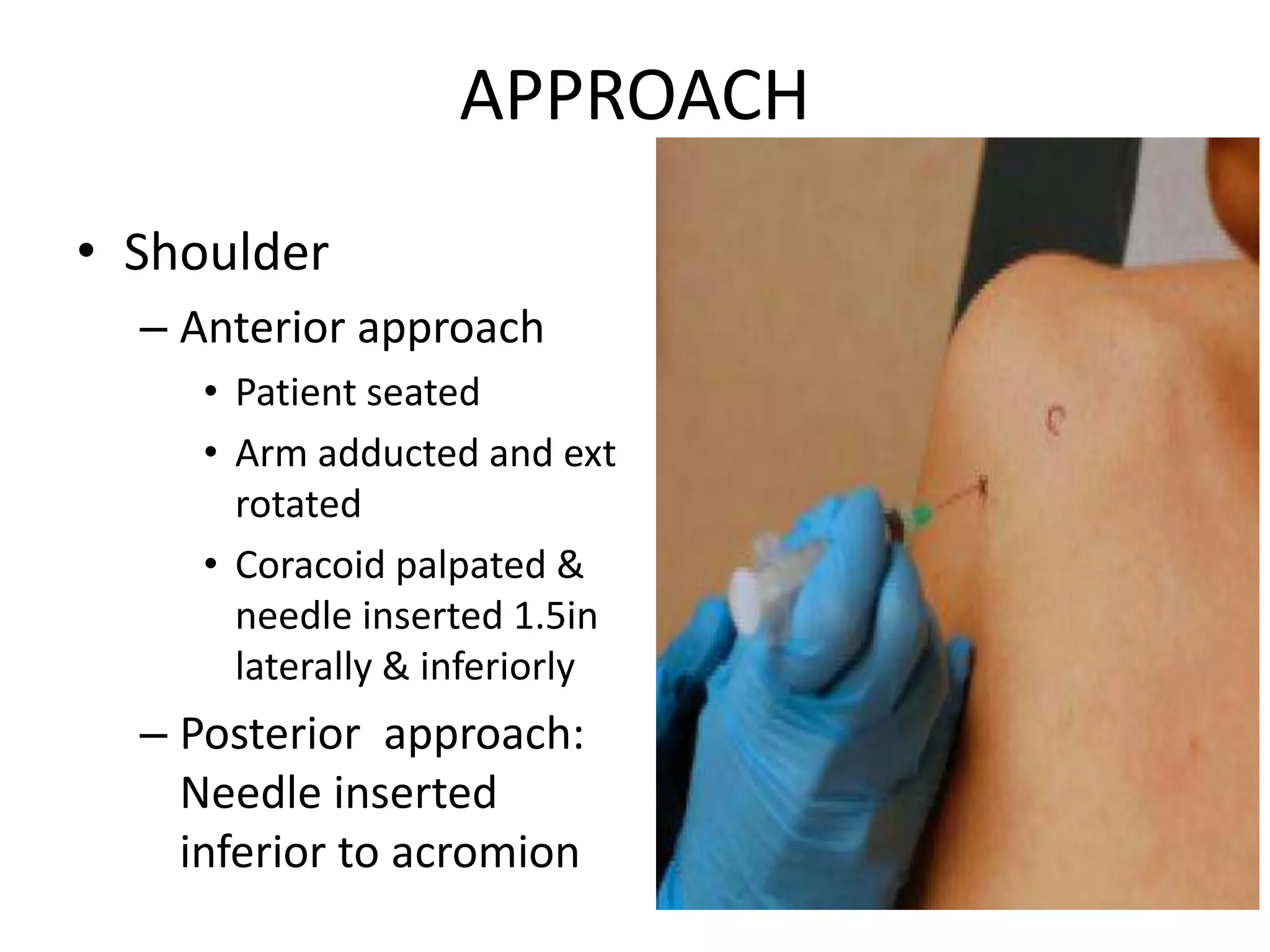
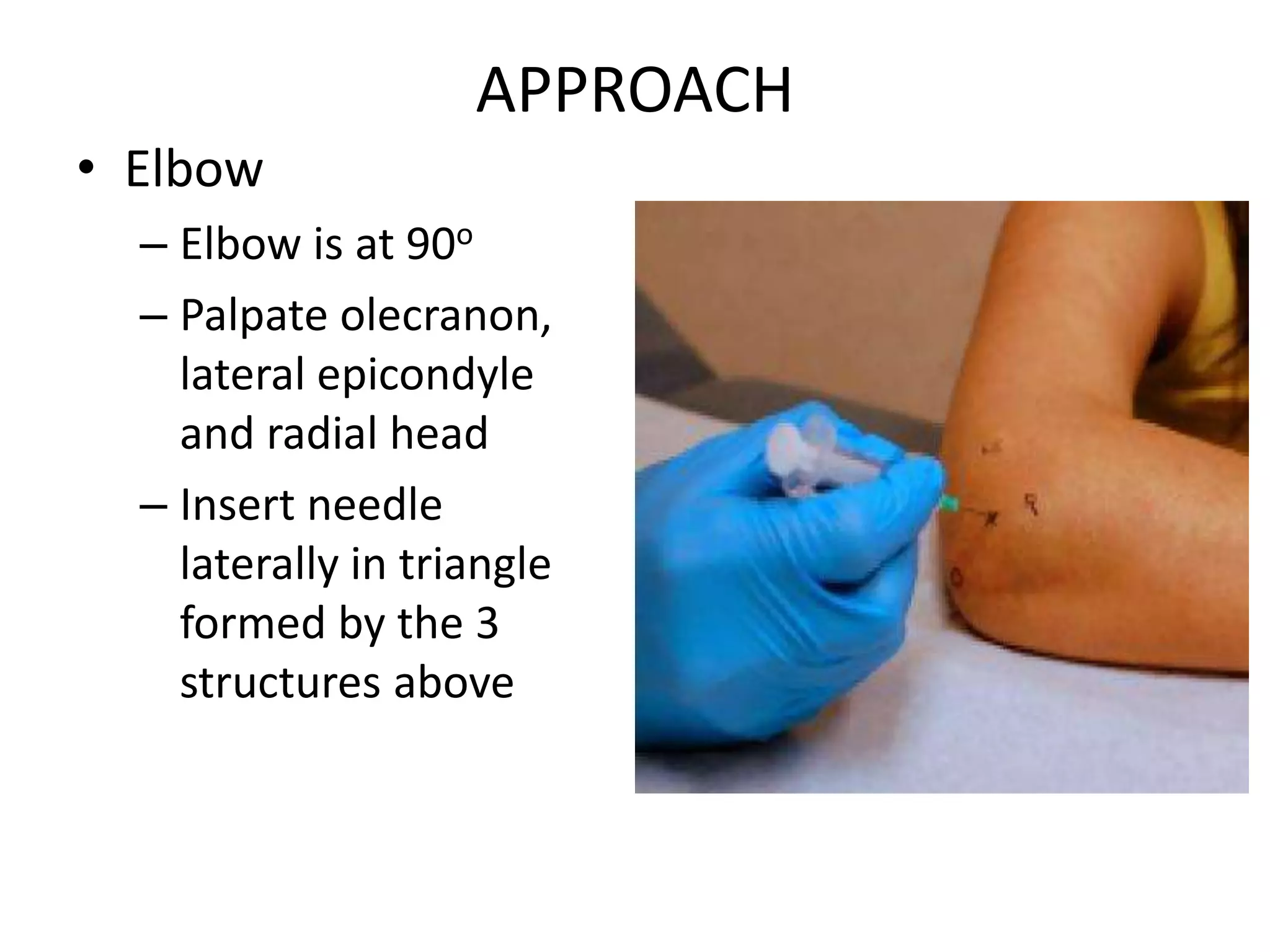
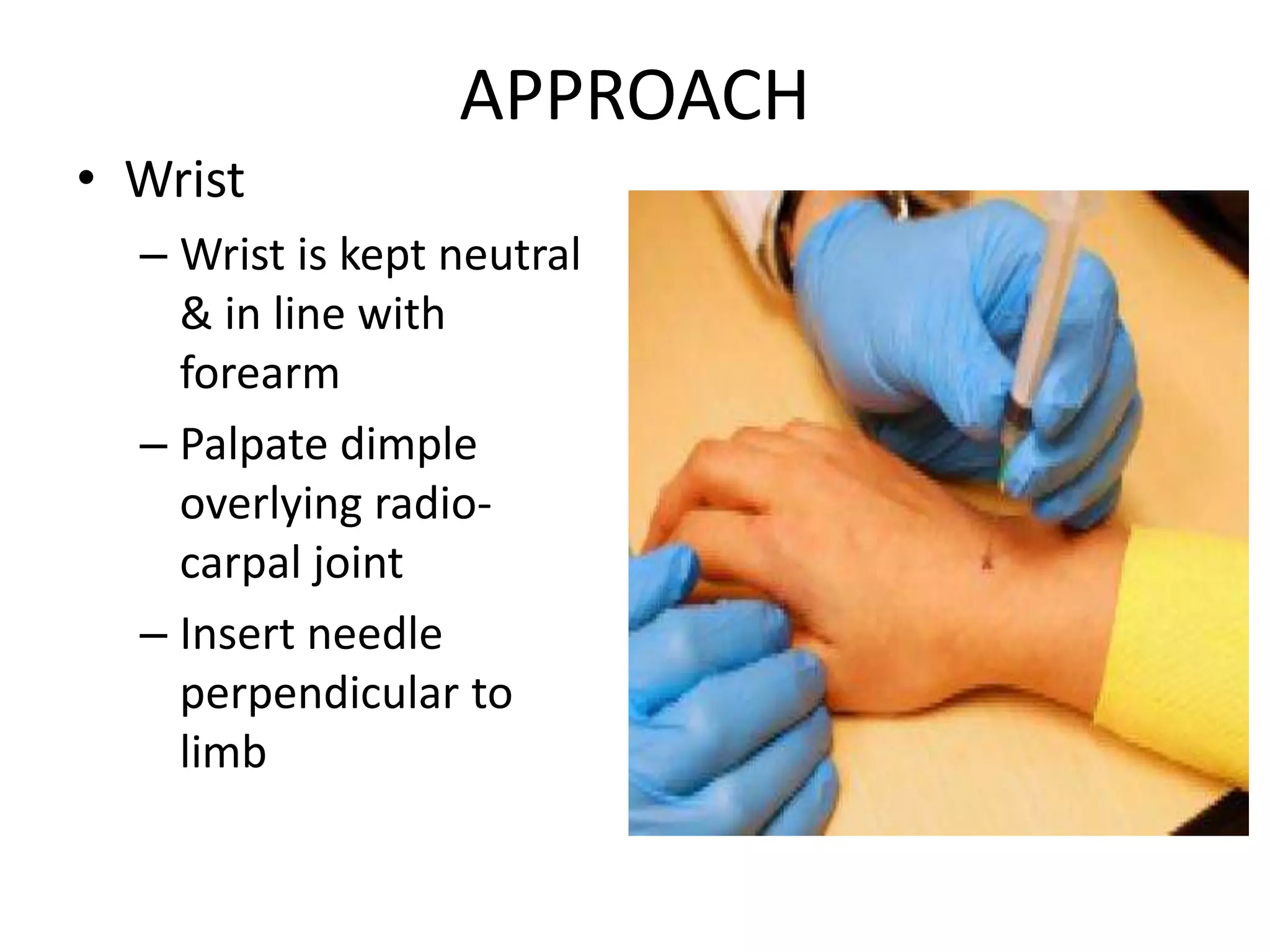
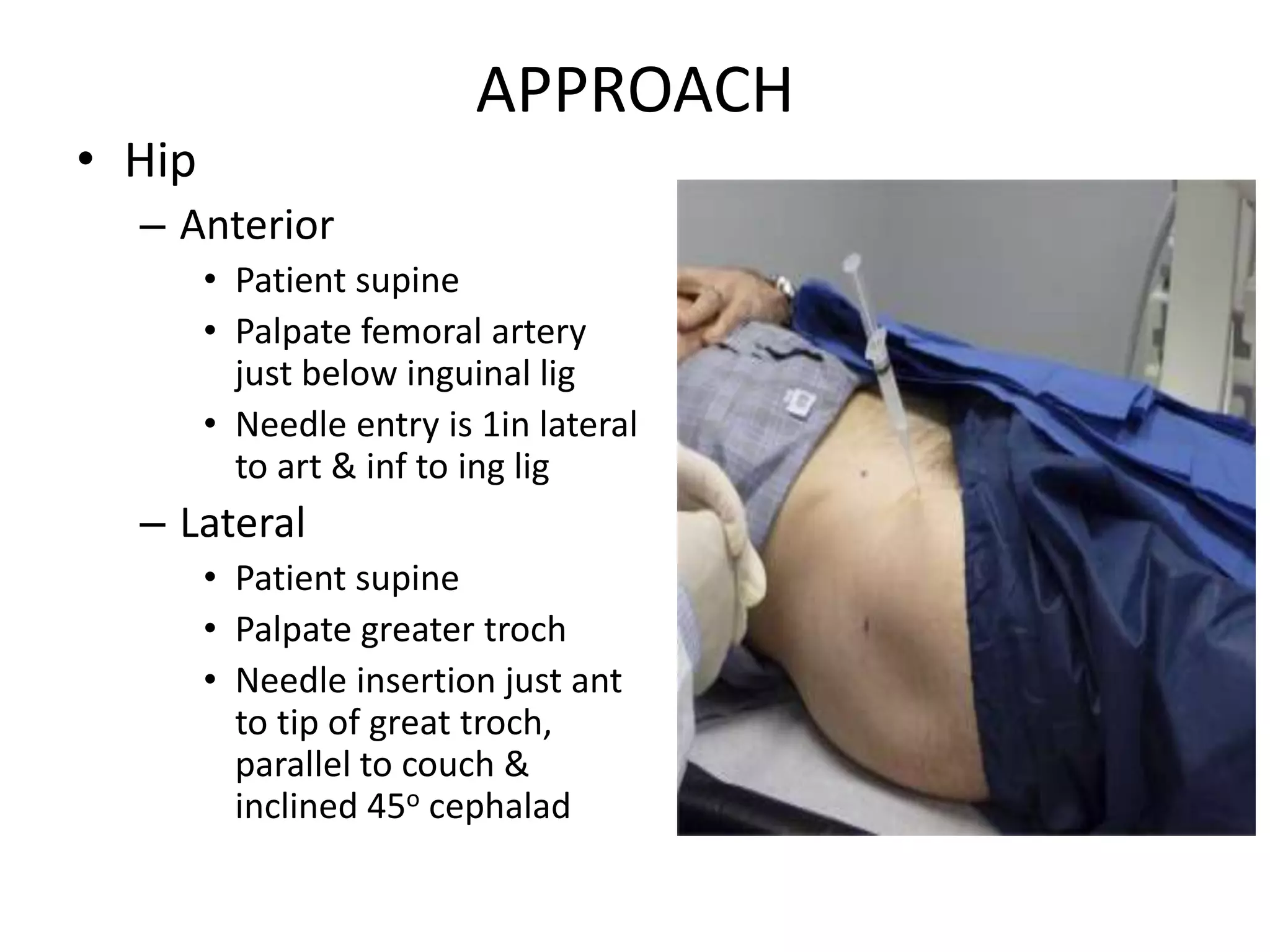
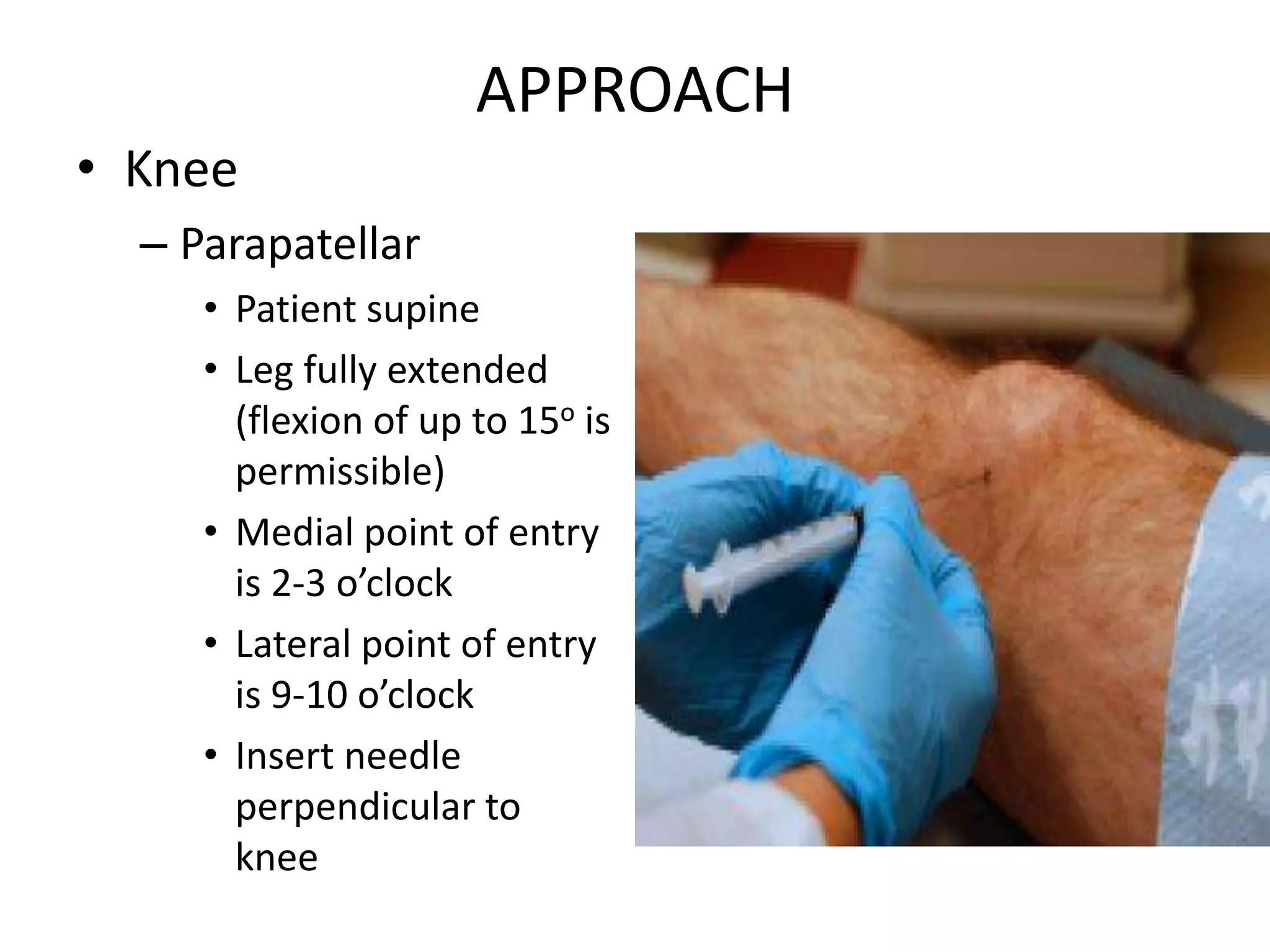
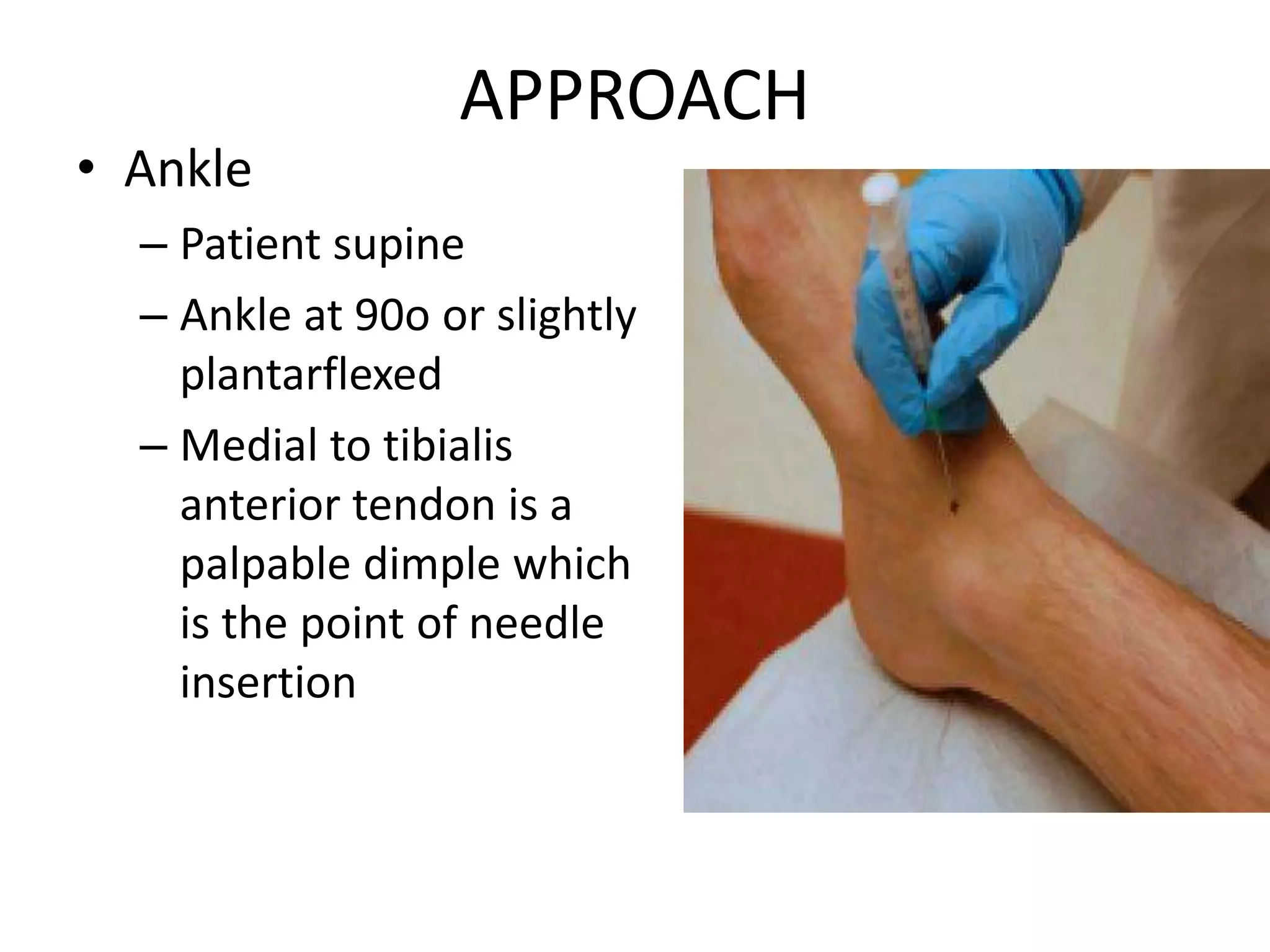
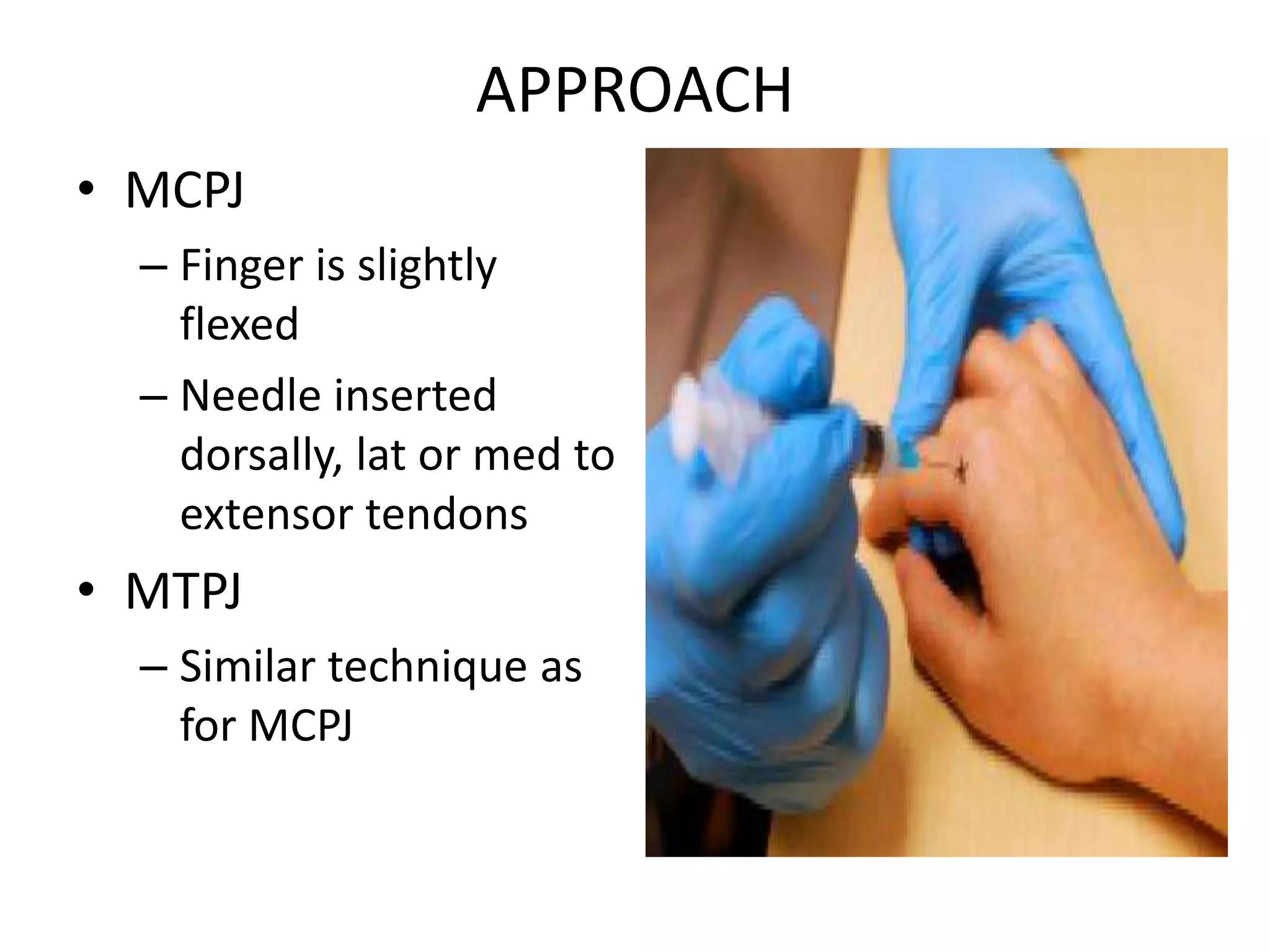
The document outlines the principles of arthrotomy and arthrocentesis, emphasizing their importance in managing joint diseases, especially in resource-limited settings. It details pre-operative to post-operative care, recommended techniques for various joints, and associated complications. Both procedures are essential for diagnostics and therapeutics in orthopaedic practice, despite advancements in minimally invasive techniques.