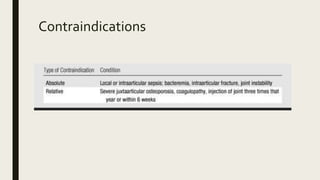
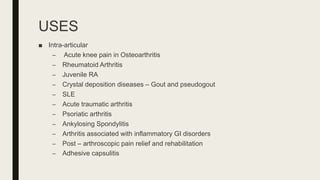
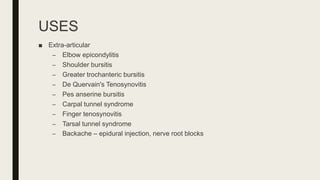
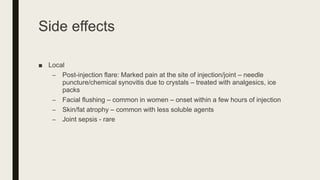
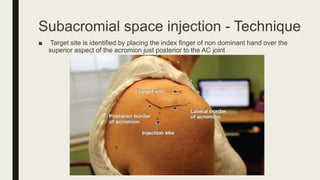
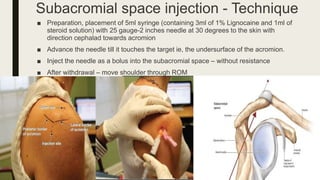
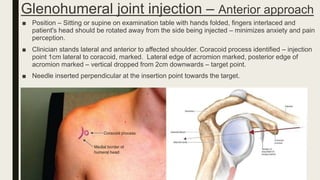
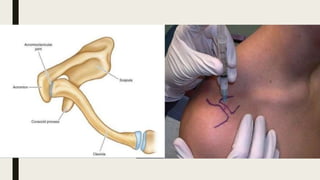
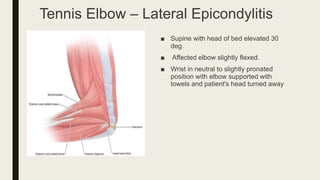
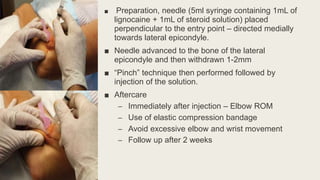
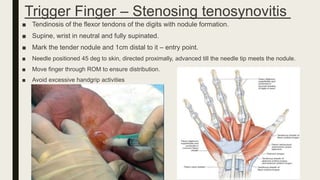
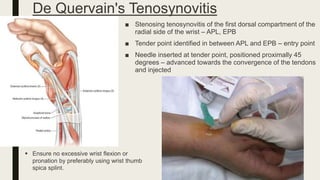
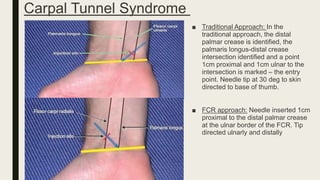
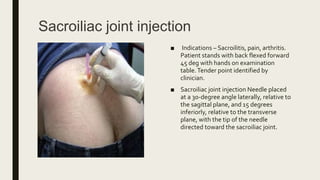
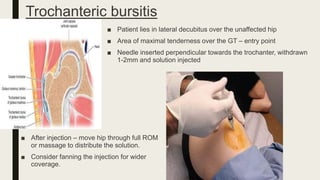
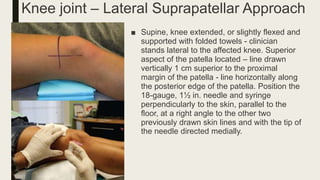
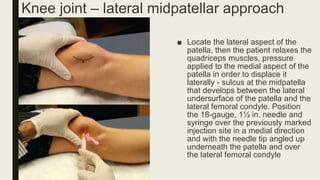
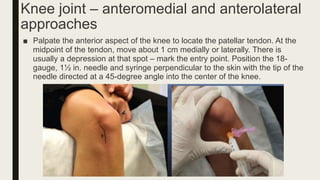
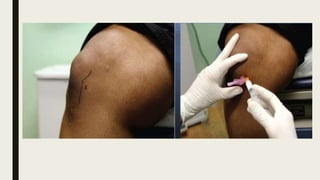
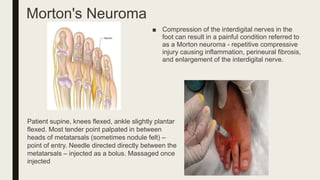
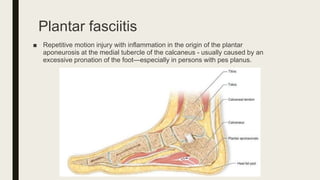
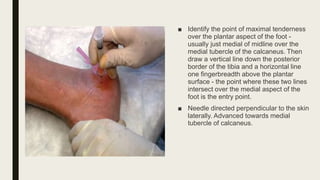
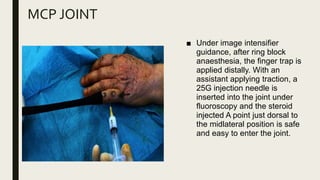
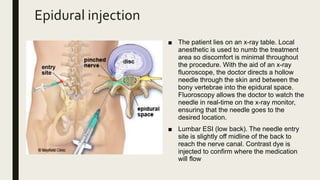
Corticosteroid injections are commonly used to treat pain conditions in orthopedics. The document discusses injection techniques for various joints like the shoulder, elbow, wrist, knee, and hip. It describes patient positioning, identifying anatomical landmarks, needle placement, and post-injection care for different approaches for each joint. The main points are that corticosteroid injections can provide local and systemic pain relief, various injection techniques exist for different joints, and precautions are taken to ensure proper needle placement and distribution of medication.