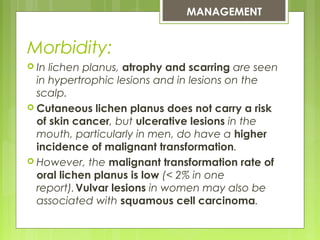
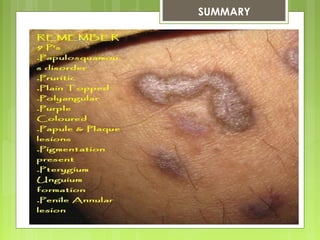
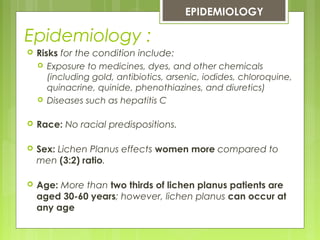
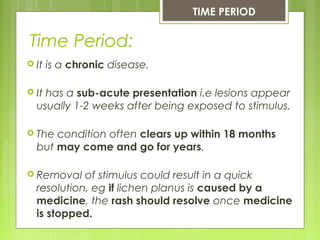
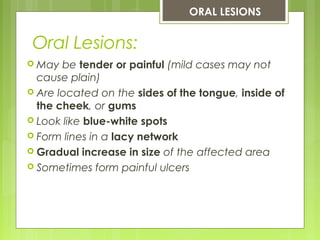
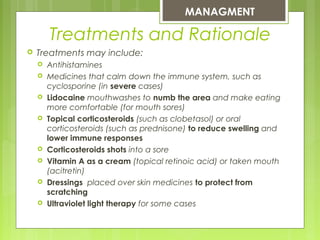
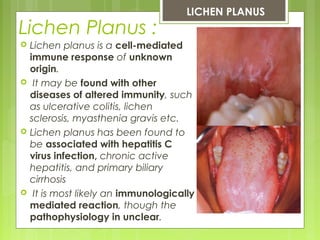
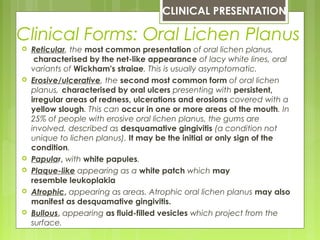
Lichen planus is a chronic autoimmune disease that affects the skin and mucous membranes. It is characterized by pruritic polygonal papules and plaques that are flat topped and violaceous. The disease commonly affects middle aged women more than men. Oral lichen planus presents as white lacy lesions inside the mouth, while skin lesions typically occur on the wrists and legs. Treatment focuses on reducing symptoms through topical corticosteroids and immunosuppressants. While usually self-limiting, oral lichen planus poses a small risk of malignant transformation over the long term.


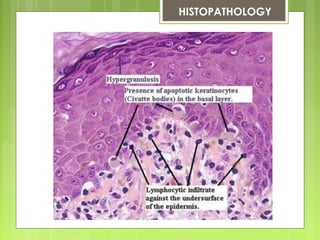
![Histopathology:
Distinguishing histopathologic features of lichen planus
include the following:
Hyperkeratotic epidermis with irregular acanthosis and focal
thickening in the granular layer
Degenerative keratinocytes (colloid or Civatte bodies) in the
lower epidermis; in addition to apoptotic keratinocytes, colloid
bodies are composed of globular deposits of IgM (occasionally
immunoglobulin G [IgG] or immunoglobulin A [IgA]) and
complement
Linear or shaggy deposits of fibrin and fibrinogen in the
basement membrane zone
In the upper dermis, a bandlike infiltrate of lymphocytic
(primarily helper T) and histiocytic cells with many Langerhans
cells
HISTOPATHOLOGY](https://image.slidesharecdn.com/lichenplanus-130910131107-phpapp02/85/Lichen-planus-21-320.jpg)